Parkinson's Disease
Parkinson’s Disease is a hypokinetic neurological disorder that leads to the degeneration of the substantia nigra pars compacta
so less dopamine is produced for the basal ganglia
💊L-DOPA- synthetic dopamine
💊Ropinirole– D2 receptor agonist
💊Apomorphine– D1 and D2 receptor agonist
💊Amantadine– blocks dopamine reuptake channel
💊Domperidone– D2 antagonist (stops nausea and vomiting by preventing dopamine activating the chemoreceptor trigger zone.
💊 Selegiline + Entacopone– drugs that allow dopamine to remain
in high quantities in the CNS, without being further
converted to other products
💊Carbidopa– dopa-decarboxylase inhibitor (prevents
dopamine leaving the CNS to the PNS)
Anxiety & Sleep Disorders
OCD, PTSD, phobias, panic, social anxiety, generalised anxiety disorders
(due to increased glutaminergic activity (treat by increasing GABA activity)

- GABAa agonists. open Cl- channels more frequently for more hyperpolarisation.
(bind at the alpha-gamma junction on the GABA channel) - Good for sedative, muscle relaxant, amnesia (surgeries)
4 Hours: Midazolam
15 Hours: lorazepam, oxazepam, temazepam
24 Hours: alprazolam, nitrazepam
48 Hours: chlordiazepoxide (lithium) diazepam (valium)
60 Hours: clonazepam, flurazepam Side Effects: confusion, drowsiness, tolerance, dependence (tremor), respiratory depression
with alcohol
(Flumazenil- used in BDZ overdose)


cause respiratory depression
- thiopental- anaesthetic
- phenobarbitone- epilepsy

antihistamines (H1), nytol, valerenic acid (valarion extract)
chlormethiazole- for elderly as no hang-over effect
Insomnia: transient -> intermediate -> chronic

Zolpidem, zopiclone (REM deficiency)
Anaesthetics 😴
General Anaesthetics enhance GABA (inhibitory = sleepy) receptors, apart from NOx which acts on NMDA (glutamate-R)

Amide Types:
- (‘i’ before the “-caine”)
- Lidocaine, Prilocaine
- metabolised in liver
Ester Types:
- (no ‘i’ before the “-caine”)
- procaine, tetracaine
- metabolised in blood

Inhaled- (maintain anaesthetic):
- isoflurane, desflurane – GABA
- nitrous oxide, xenon, ketamine
- block NMDA (non-competitive), so Ca2+ cannot carry the pain signals to the post-synaptic neurone
- thiopentone, propofol, etomidate
- keep GABAa open for hyperpolarisation of post-synaptic neuron
Huntington's Disease
Huntington’s Disease occurs due to degeneration of the indirect pathway & overstimulation of dopamine receptors which cause hyperkinetic movement



Parasympathetic Nervous System
Parasympathetic nervous system works on muscarinic (Ach) receptors
Muscarinic Agonist

Muscarinic Antagonist


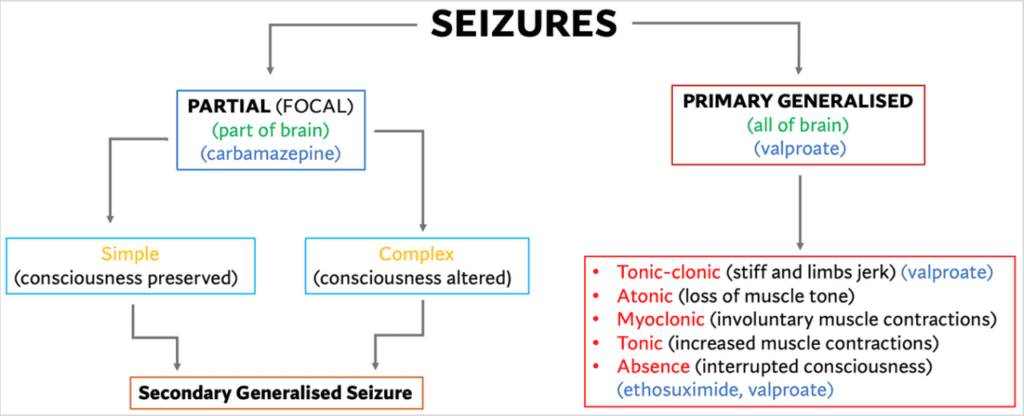
Epilepsy
- Epileptic Seizure- a seizure resulting from epilepsy (excess activity of
neurones in the brain) - Epileptic Disorder- chronic neurological condition characterised by
recurrent epileptic seizures - Seizure- sudden, short event involving a change in a person’s awareness of
where they are or what they are doing, their behaviour or feelings. - Status Epilepticus = seizure longer than 5 minutes (treat with lorazepam)
To treat epilepsy, need to dampen neuronal hyperexcitability (reduce
excitation/ increase inhibitory influences)
- a ketogenic diet may help children who have epilepsy








unipolar depression & bipolar
Characterised by:
- Dysphoria (low mood)
- Anhedonia (lack of positive feelings)
Can be treated with:
- Electroconvulsion Therapy- non-responsive depression (controversial therapy due to misuse histroically)
- Lithium and ketamine
💊 Tricyclic Antidepressants (TCAs):
- imipramine, amitriptyline, clomipramine
- block 5HT and noradrenaline (NA) reuptake transporters
- 2-3 weeks to take effect
- not a very selective drug
- Cardiotoxic
💊 Selective Serotonin Reuptake Inhibitors (SSRIs):
- sertraline, fluoxetine, citalopram
- blocks 5HT reuptake transprters (SERT) (safe in overdose)
💊 Selective Noradrenaline Reuptake Inhibitors (SNRIs):
- venlafaxine, maprotiline
- blocks NA reuptake transporters (NET)
💊 Monoamine Oxidase Inhibitors (MAOIs):
- phenelzine
- inhibit MAO, so monoamines can remain in high quantities in the synapse
- Side effect: Cheese Reaction- consuming foods with high tyramine
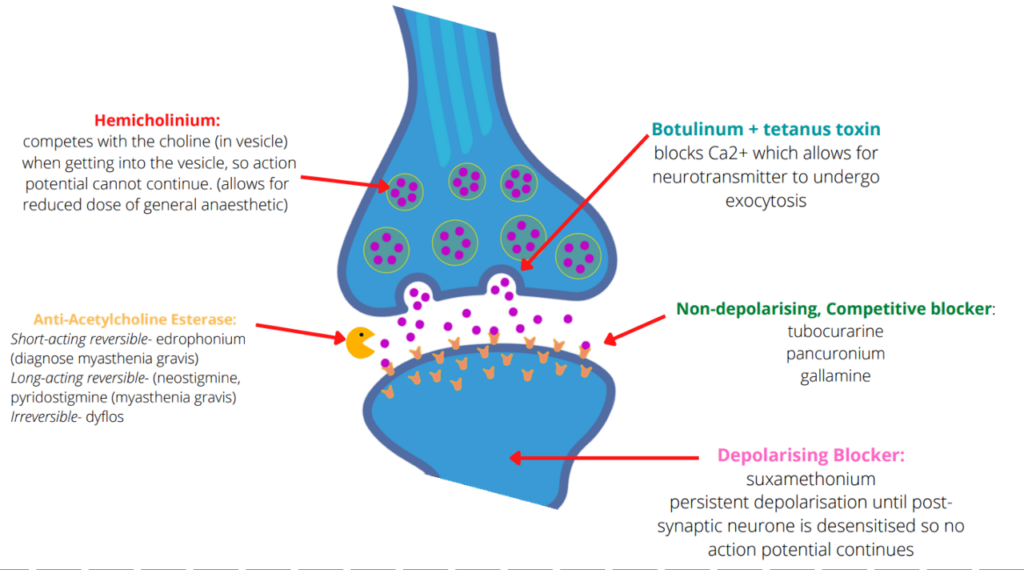
neuromuscular junction (NMJ)
Pain
Pain can either be
- Inflammatory – as a result of tissue damage 🙁
- Neuropathic – pain neurones being overactive (this pain tends to be chronic)

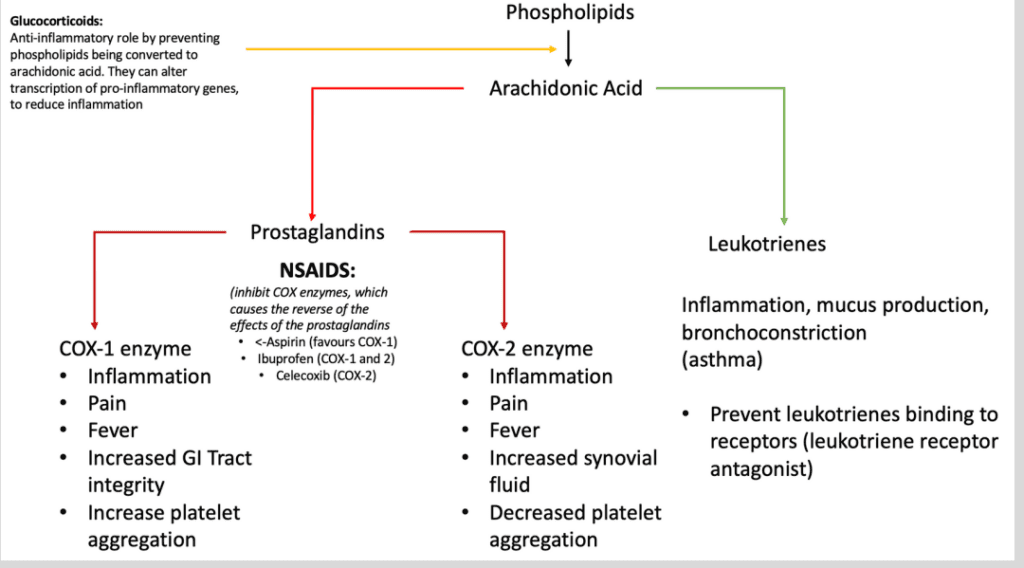
NSAIDS
- Aspirin (COX-1 inhibitor)
- ibuprofen (COX-1 inhibitor)
- diclofenac (COX-2 inhibitor)
Steroids (SAIDS)
- hydrocortisol, cortisone
- (block conversion of phospholipids to arachidonic acid)
Triptans
- sumatriptan (‘-triptan” used for headaches and migraine
- inhibit 5HT receptors vasodilation

- Na+ channel blockers- carbamazepine
- Ca2+ channel blockers- gabapentin, pregabalin
- NMDA blockers-
- ketamine (extreme pain)
- antidepressants
Opiates
- Mu, delta, kappa receptors.
- Mu- opiates
- Mu receptors- morphine, codeine, fentanyl (mimics endorphin,
opens K+ channels, hyperpolarising the post-synaptic neurone,
so pain signal cannot continue)
- Mu receptors- morphine, codeine, fentanyl (mimics endorphin,
- Mu- opiates
- delta- enkephalins
- kappa- dynorphin
💊 naloxone- opiate antagonist (give for overdose)
Others:
Paracetamol. (in overdose, treat with activated charcoal in first
hour, then use acetylcysteine) (can lead to hepatotoxicity)
Anti-pyschotics
Schizophrenia- excess dopamine (so give dopamine antagonists). Leads to positive (auditory/visual hallucinations) and negative symptoms (withdrawal, lack of pleasure)
Typical Antipsychotics:
- chlorpromazine (aplastic anaemia)
- flupenthixol
- haloperidol
- D2 antagonists, targets positive symptoms
- Side effects: movement disorders (extrapyramidal symptoms), hyperprolactinaemia
Atypical Antipsychotics: (first-line)
- clozapine (agranulocytosis)
- risperidone
- olanzapine
- D2 and 5HT antagonists, targets positive and negative symptoms
- same side effects as typical antipsychotics, but less severe, + weight gain
Aripiprazole: (third generation)
- D2 agonist,
- 5HT1a agonist, 5HT2a antagonist
- targets positive and negative symptoms and hallucinations
- side effects: weight gain, hyperprolactinaemia. Much less EPS side effects 🙂
Neuropharm, NMJ, P450