OCaPE: NSB #8
OCaPE: NSB #8
Muscle weakness & twitches
A patient has come back from holiday and comes in complaining of having difficulty carrying out movements and describes “weakened muscles”. The patient also mentions they have been having annoying twitches in their left arm.
5 minutes
Q1)
What is the name of the test you would use to elicit a muscle reflex to further diagnose this patient?
Tendon tap reflex (1)
AKA Deep Tendon Reflex/ Myotatic Reflex/ Muscle Stretch Reflex
AKA knee jerk or biceps stretch
Describe how you would carry out this test and what myotome you are testing ?
Either of the following (5 marks):
BICEP
- Patient has straightened arm,
- place your thumb over the tendon area.
- Hit with tendon hammer
- Biceps should contract, (elbow joint should pull back)
- forearm should flex (rotation)
- You are testing C5-C6
OR KNEE JERK REFLEX
Strike below the patella with tendon hammer
Tap briskly
Lower leg should extend outwards
L3-L4 (L3/L4 kick the door)
What fibres are responsible for this reflex and what is their role?
1a afferents.
These report dynamic changes – e.g. report velocity of length change. Maintain length of spindle via muscle stretch reflex (monosynaptic activation of motor neurones) .
Stabilises the muscle (3)
The patient has a weak tendon tap reflex. What is this symptom called?
Flaccid paralysis (LMN signs) (2)
You take the following lab tests.
HbA1c: 4%
Hb : 13.5g/dL
Anti-AChR Ab : Negative
Anti-ganglioside antibody: negative
WBC: 718
CSF
Appearance: Clear
Combining the above results with the symptoms and weak tendon tap, what is the most likely diagnosis?
Must give correct diagnosis with explanation for (4 marks)
- Poliomyelitis – due to high WBC (infection)
- Polio grows in the spine and can kill a motoneurones, leading to flaccid paralysis
- anti-achr-ab negative rules out myasthenia which can also cause LMN signs .
- Negative for anti-ganglion antibodies suggests it is not guillan-barre syndrome
Three days later, the patient has symptoms of a fever, vomiting, a stiff neck and hurts when looking at light. Explain the pathology?
Patient has developed meningitis.
Polio can also cause (viral) meningitis (2)
Label the three layers of the meninges below
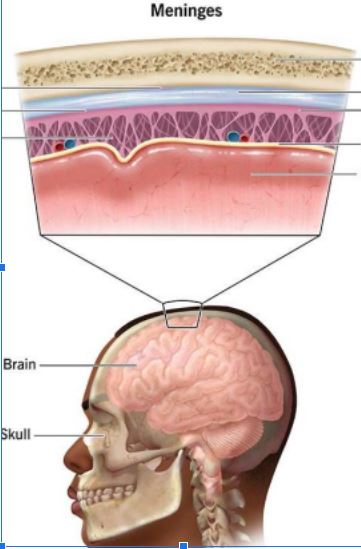
From top to bottom (scalp to brain):
Dura, Arachnoid, Pia (2)
Describe how polio can be prevented?
Live oral polio vaccine (1)
- Produces IgA & IgG
- Attenuated via tissue