Notes: NEUROANATOMY NUCLEI SUMMARY
Notes: NEUROANATOMY NUCLEI SUMMARY
Don’t know your aunts from your peduncles? Your feta from your olives? This page is for you.Best viewed on big screens
Waffle Warning !
You may not need to know all the locations or exact 3D structure of every one of the nuclei here, some diagrams are just to help you better picture stuff
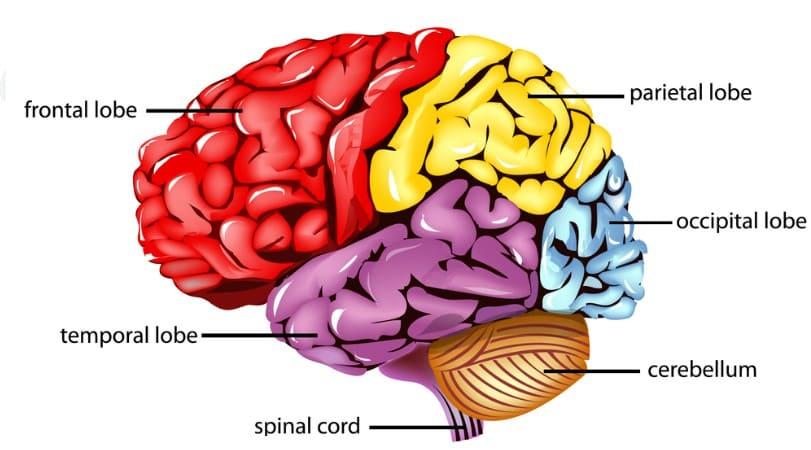
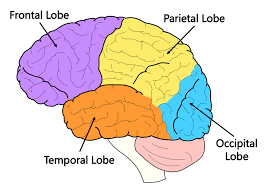
Cerebrum
The cerebrum is the main bit you think of when you think of the brain.
Made of lots of:
-Sulcus : ridges
-Gyrus: the big bits of grey matter
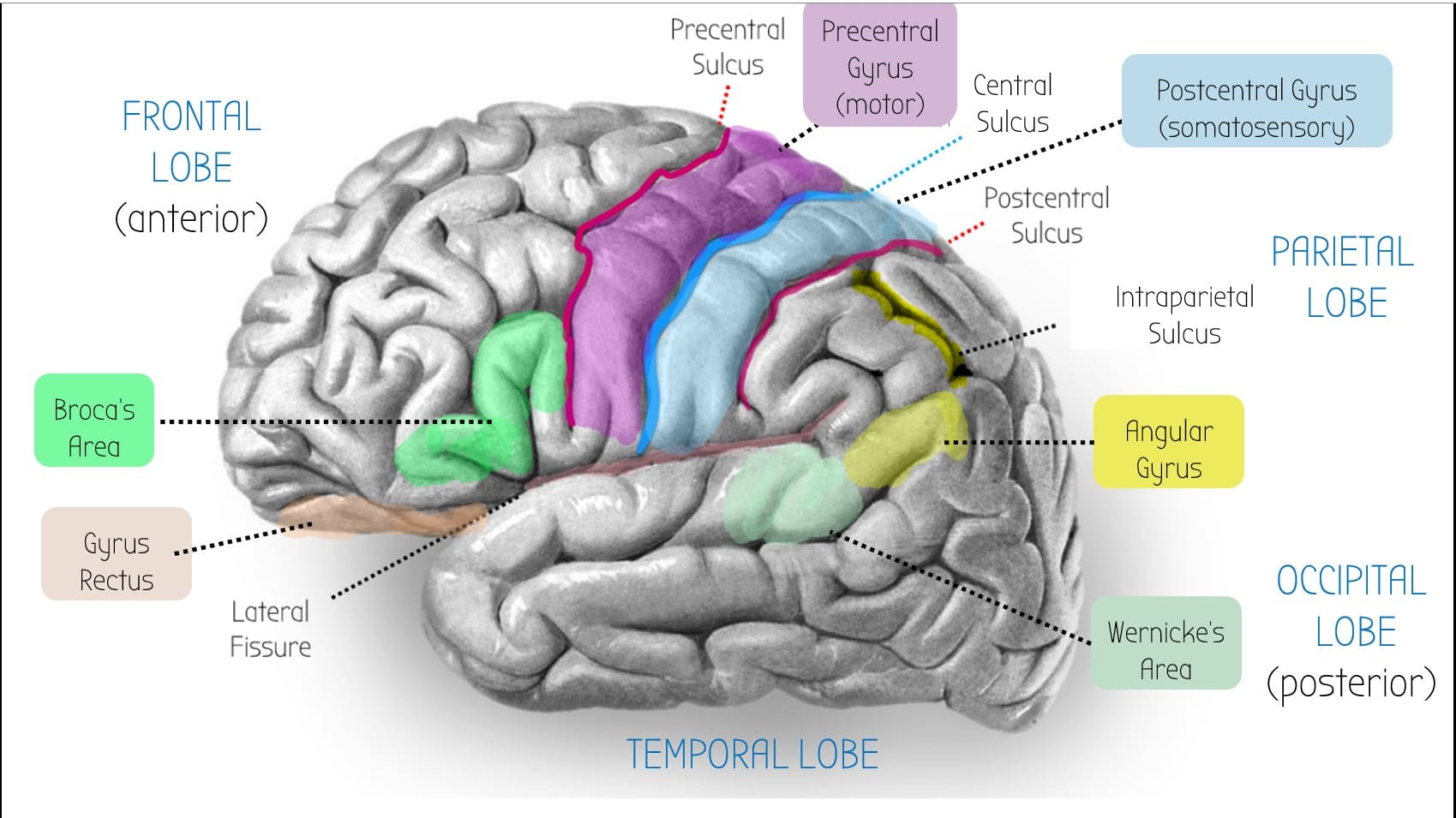
Angular Gyrus
--> Helps with reading & language
Wernicke's Area
-> Language understanding centre.
--> Only found in the dominant hemisphere of the brain (usually the left side)
Broca's Area
-> Motor speech area
--> Only found in the dominant hemisphere of the brain (usually the left side)
--> Stroke: won't be able to say words
Parietal lobe
--> Dominant side (usually left hemisphere): wernicke's area, broca's area, angular gyrus: language stuff
--> Non-dominant side (usually right hemisphere): spatial processing e.g. constructional ability
Intraparietal Sulcus
--> Contains cool neurones that respond to specific numbers.
--> Important for maths and counting
Postcentral Sulcus
Important area for stereognosis - the ability to recognise objectts by tthier shape and texture
Receives info from DCMLT (discriminative touch)
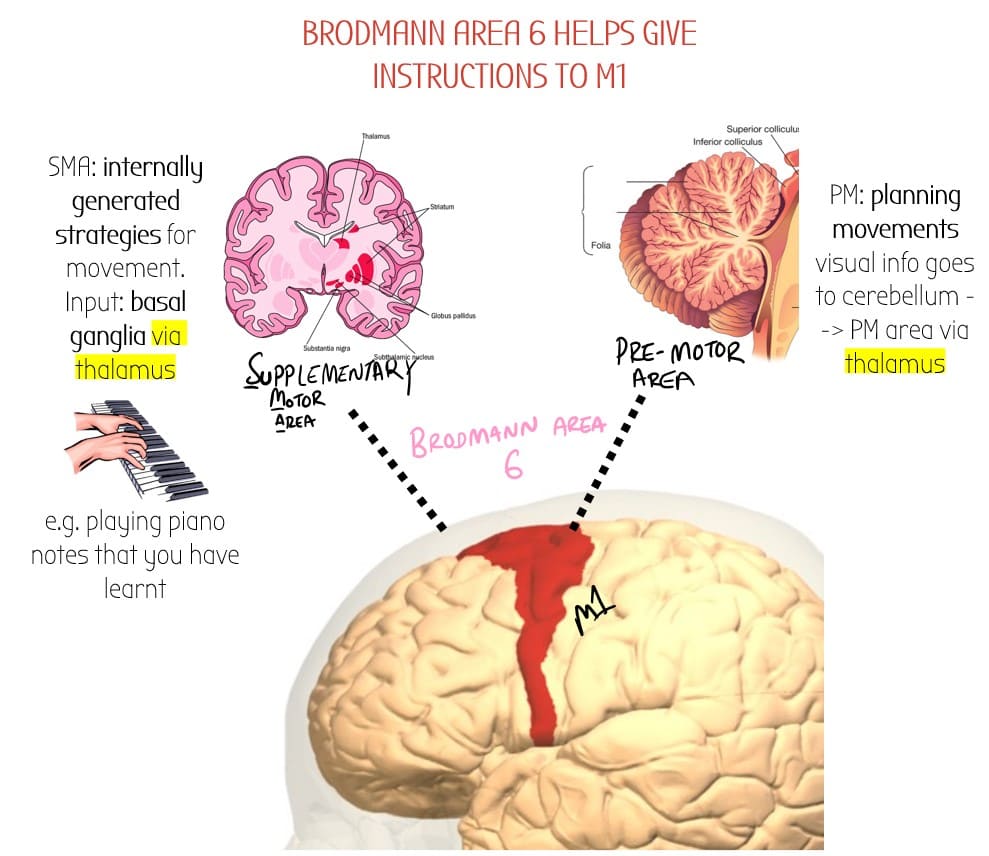
Brodmann area 6
Just anterior to M1 is Brodmann area 6 - an area which assists with motor control.
It is split into:
- Supplementary Motor Area (SMA)
- Premotor Area (PM)
Precentral Gyrus
M1 Motor Cortex.
Main motor cortex - inputs : ventral lateral (VL) nucleus of thalamus
Outputs: Corticospinal tracts
Postcentral Gyrus (S1)
-Main somatosensory area
-inputs: medial leminscus (conscious proprioception) & spinothalamic tract (nociception)
Lateral Fissure
AKA sylvian fissure
Auditory Cortex buried here.
Superior Parietal Lobule
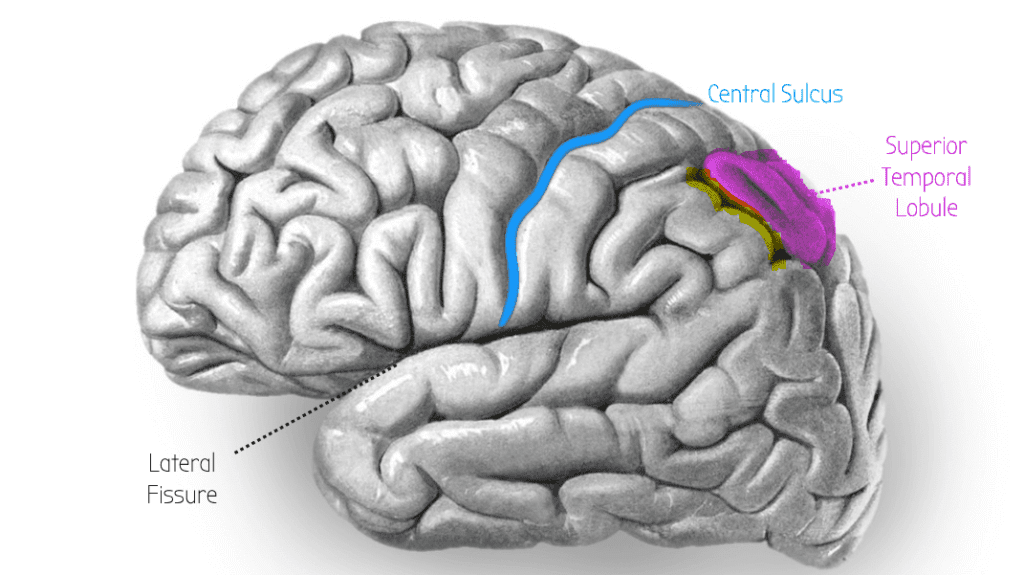
👀 Visual processing - WHERE OBJECTS ARE
--> Info comes from main visual cortex V1 (occipital lobe)
Bit of Cerebrum
Location
Function
Connections & Neurotransmitters
Pathologies
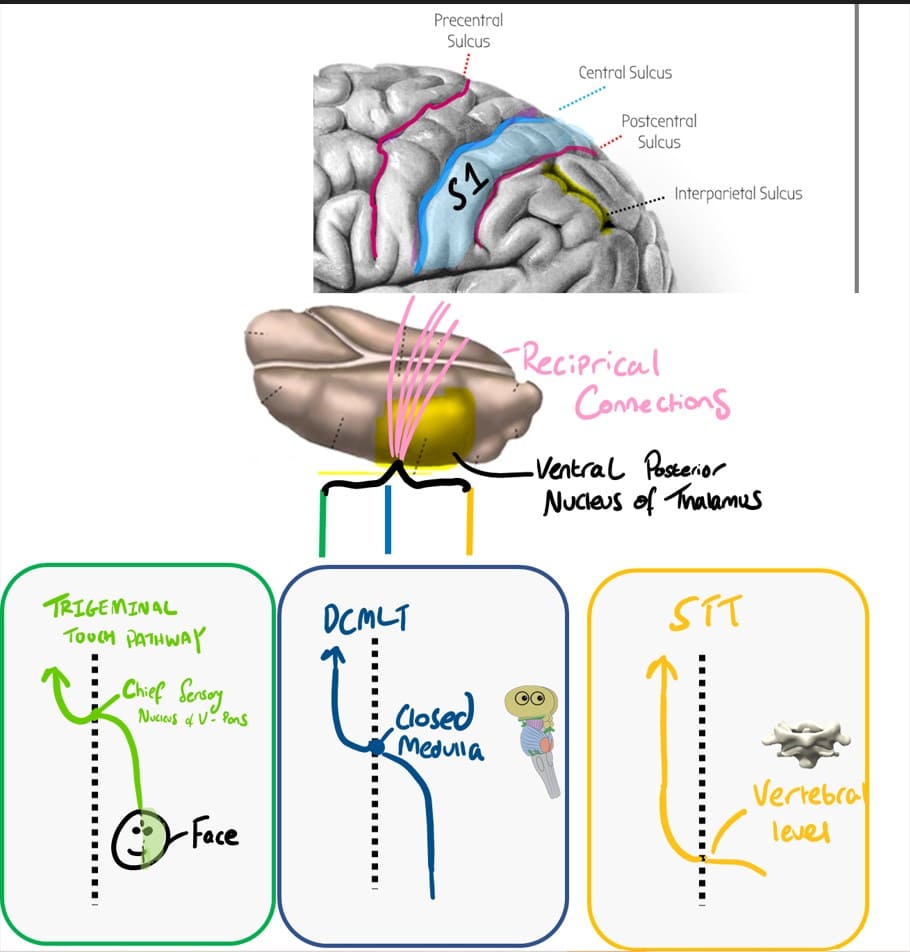
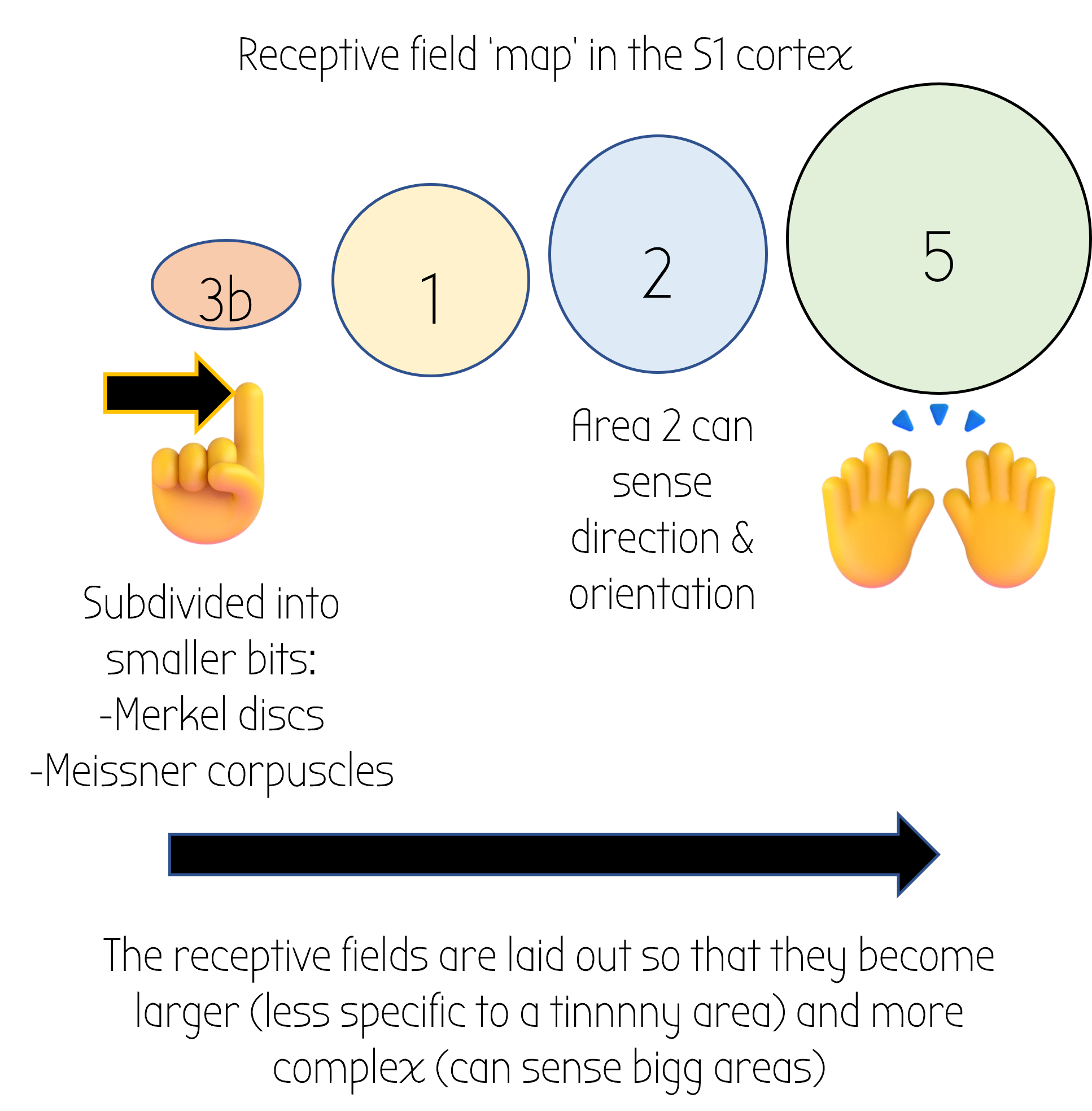
Post-Central Gyrus S1
Posterior to the central sulcus
Somatosensory processing area – S1
- Like most of the cerebrum (cortex), S1 is made up of 6 layers
- Just like the motor cortex, the somatosensory gyrus remembers where certain sensations came from – this is called a receptive field map
- The receptive field map is divided into 4 areas which go from tiny (point on a finger) to big (both hands)
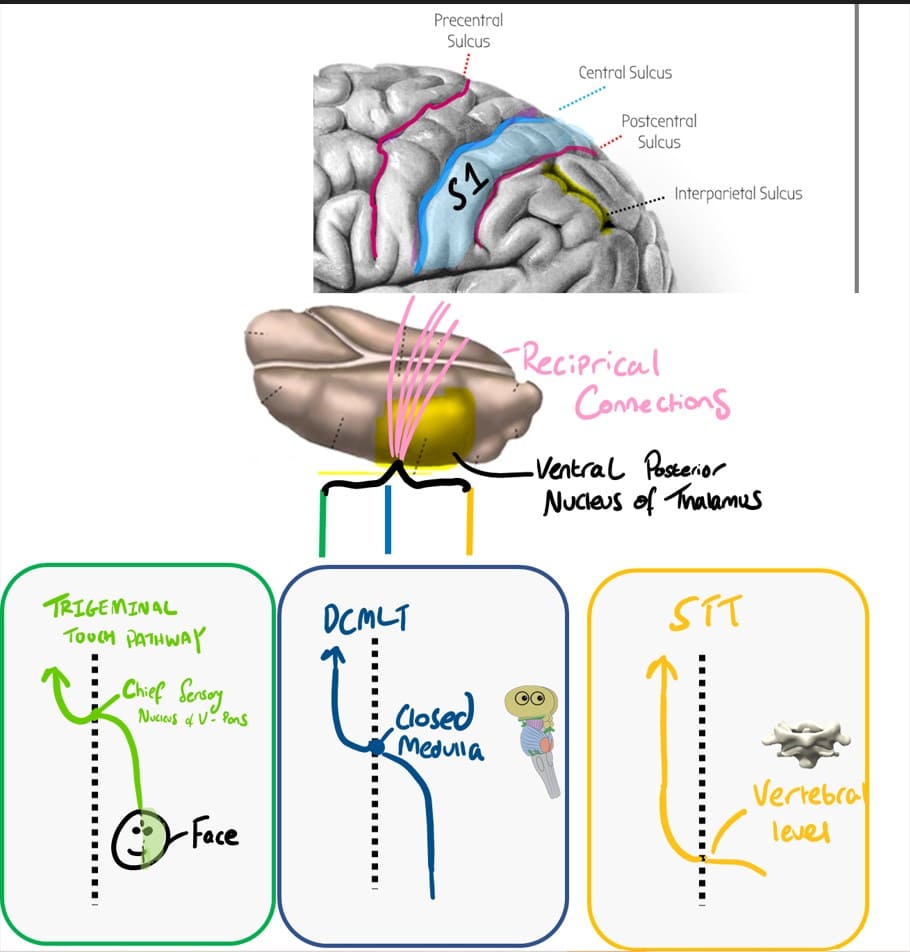 INPUT: TRACTS VIA VP NUCLEUS OF THALAMUS
INPUT: TRACTS VIA VP NUCLEUS OF THALAMUS
Several tracts. These first go to the ventral posterior (VP) nucleus of the thalamus and then go to S1 via reciprocal connections.
e.g.
- DCMLT – dorsal column medial lemniscus – conscious proprioception
- Spinothalamic tract – nociception
- Trigeminal touch pathway – column pathway for the face. Fibres project to trigeminal principal sensory nucleus, cross at the midline
-MCA stroke – contralateral loss of sensory info
Precentral Gyrus M1
Anterior to central sulcus
Makes up the M1 motor cortex
INPUT:
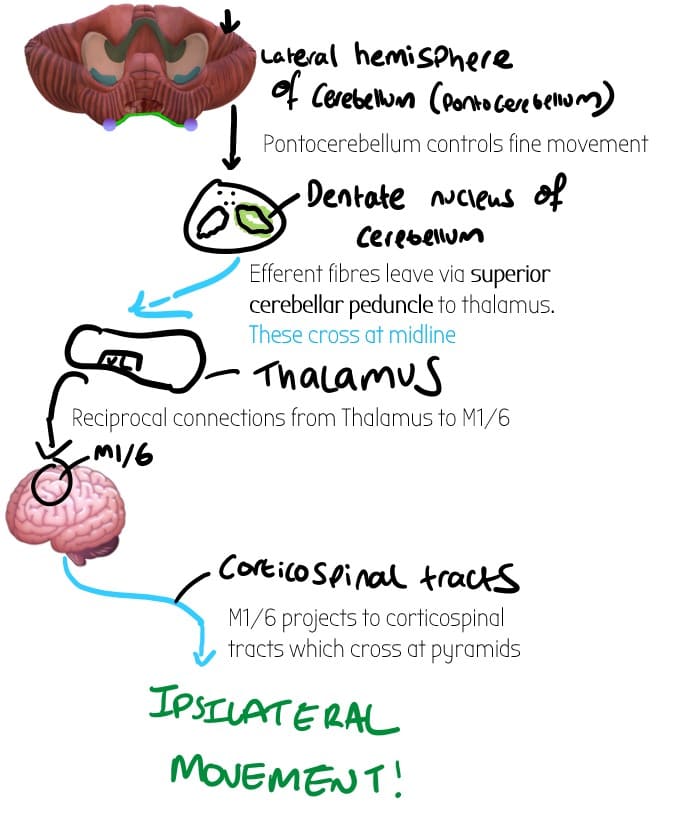
Pontocerebellum (lateral bits of cerebellum) –> dentate nucleus in cerebellum via the Ventrolateral thalamus:
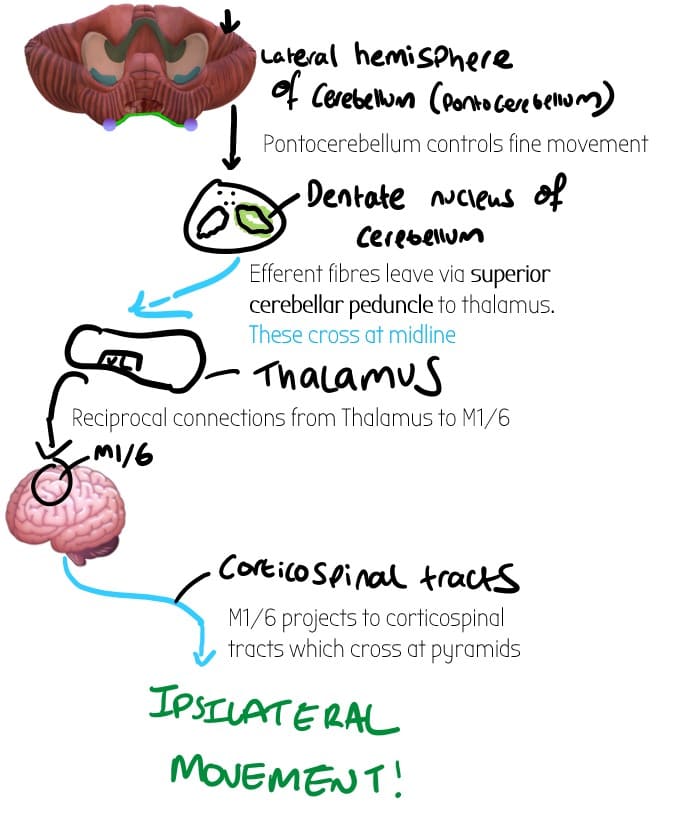
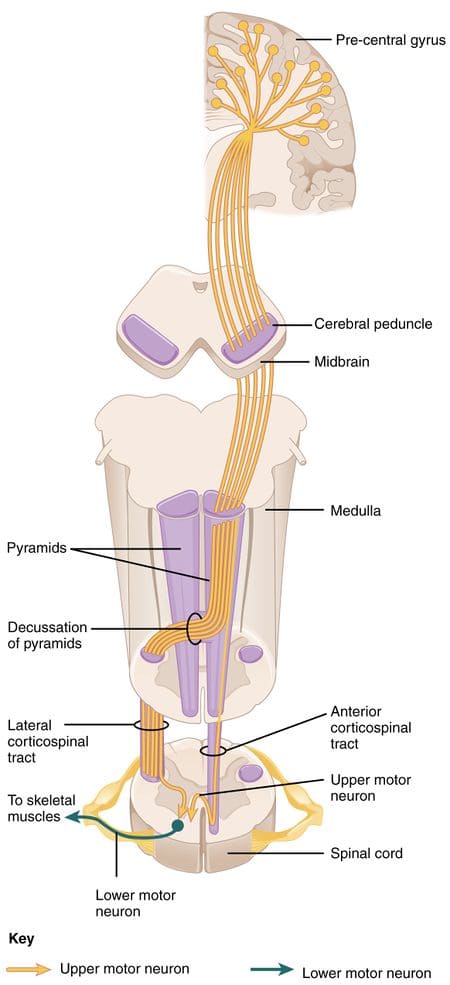
OUTPUT: Corticospinal tracts – cross at pyramids = contralateral
–> Contralateral movement from the M1 (but ipsilateral if you trace all the way to the cerebellum). – Audio explanation below:
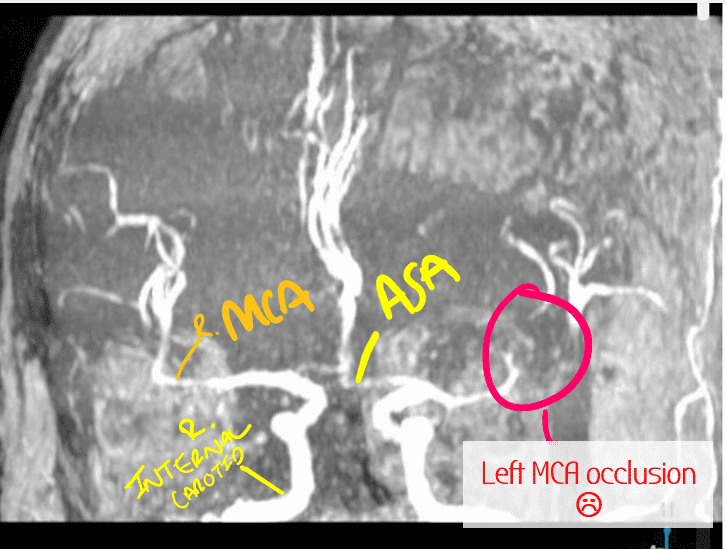
-MCA stroke:
-can’t move opposite side of body. The MCA affects face most = conttralateral hemiplegia of face
Brodmann Area 6
Just anterior to the M1 precentral gyrus
Assists in motor control
-divided into supplementary motor area
-premotor area
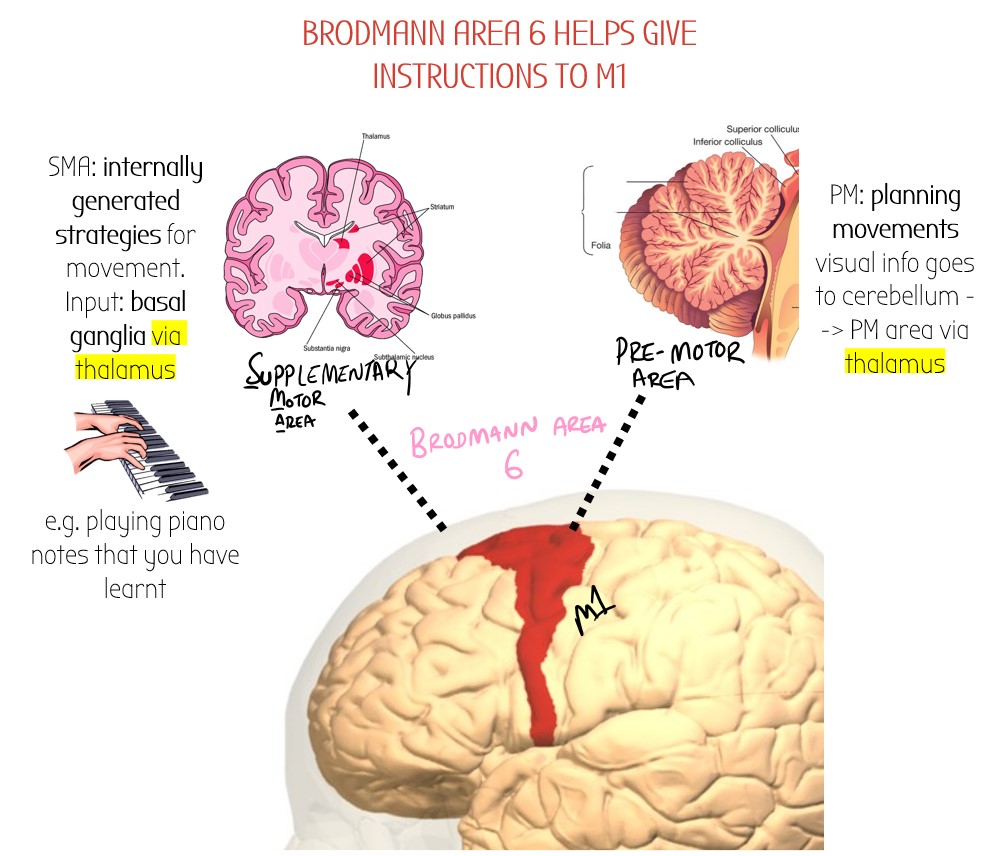
INPUTS:
-Lateral parts of cerebellum (Pontocerebellum) –> dentate nucleus (DCN) –> Ventral Anterior Thalamus –> Area 6
-MCA stroke
Parietal Lobe
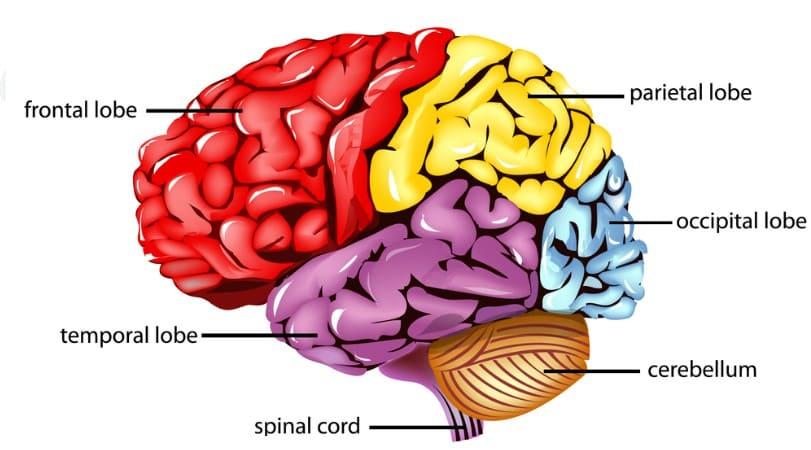
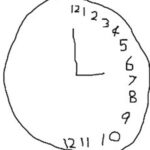
Non-Dominant side (usually right hemisphere):
Spatial reasoning
- Right parietal lobe is also responsible for body image. Lesion = you dont recognise your own hand as yours!
- Constructional ability– Make stuff. Lesion = cannot put 3 -piece jigsaw puzzle together
- Lesions in R lobe can also lead to hemineglect – you brain just doesn’t see one side of the world as being there – spoooky!
This makes patients draw stuff like this:
Connections & Neurotransmitters
-MCA stroke
Broca's area
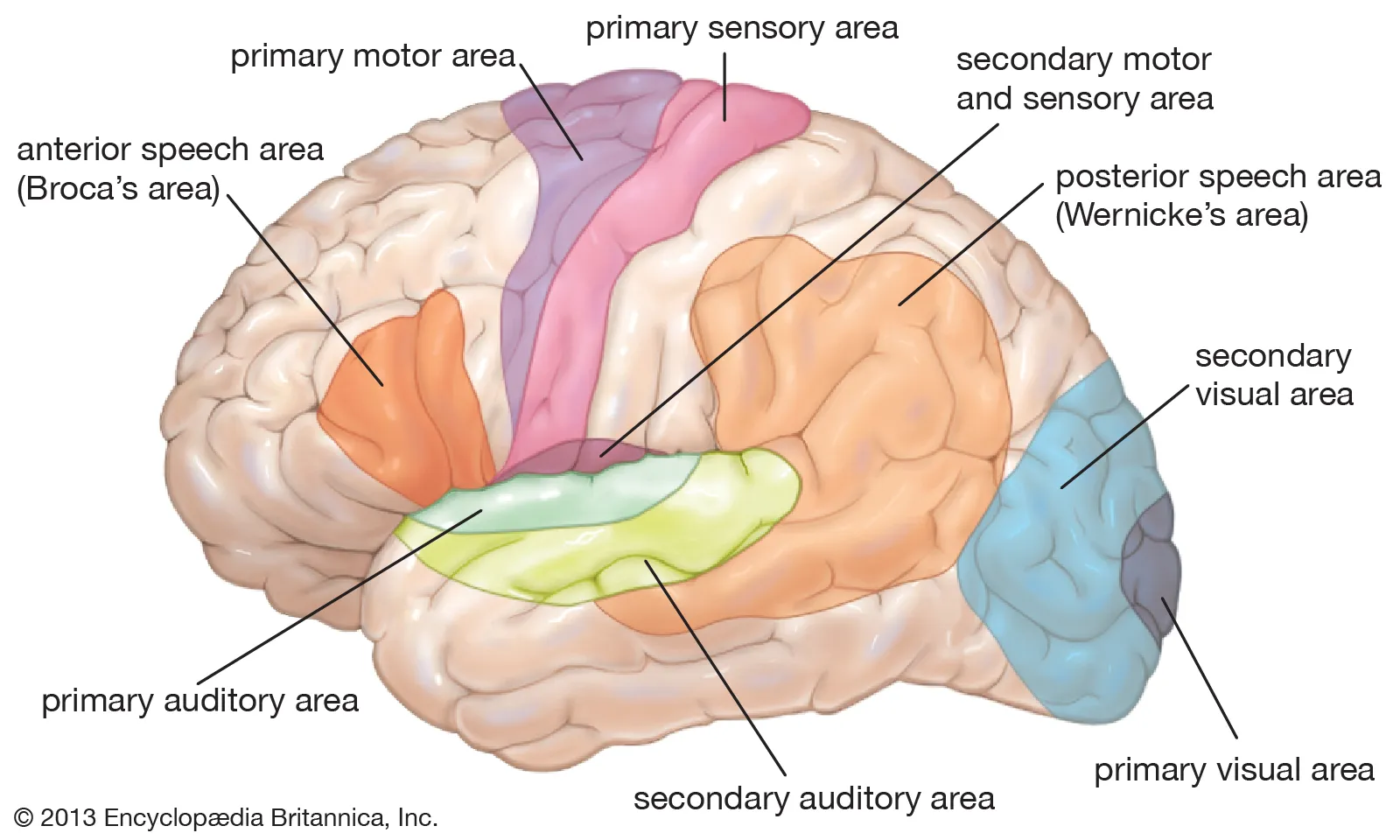
Dominant frontal lobe (shown in orange)
Motor speech ara at dominant side
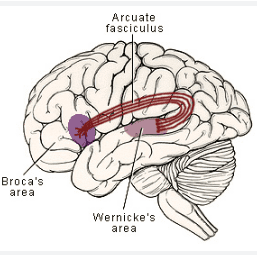
Connected to the wernick’es area by fibres called the arcuate fasiculus
🩸 Supplied by superior division of MCA
MCA Stroke in Broca’s area = expressive aphasia:
-speech is very reduced with limited vocab
-very hard to make out proper sounds- speech is very jumbled
Werncike's Area
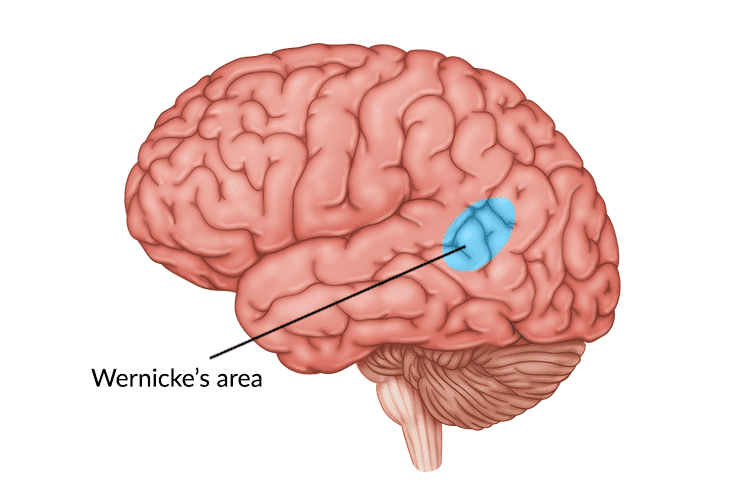
Dominant (usually left) temporal lobe
Language area of speech – chooses the correct words to say etc
Connected to the Broca’s area by fibres called the arcuate fasiculus
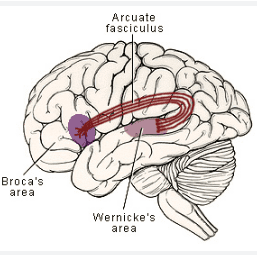
Also connected to auditory cortex to help understand sounds

MCA Stroke in Wernicke’s area = fluent/receptive aphasia:
-Words come out and can be heard but they don’t make any sense
-Words are random like a word salad.
-Also patient may struggle to understand words – poor comprehension 🙁
Arcuate Fasiculus
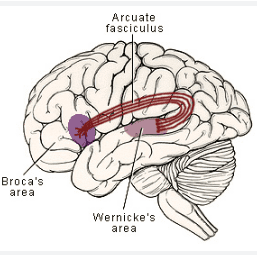
Parietal lobule
Connects both the speech areas: Broca’s (anterior) and Wernicke’s (temporal lobe)
Connects Broca’s & Wernicke’s area together

Can understand and speak well BUT difficulty in repeating words
=CONDUCTION APHASIA
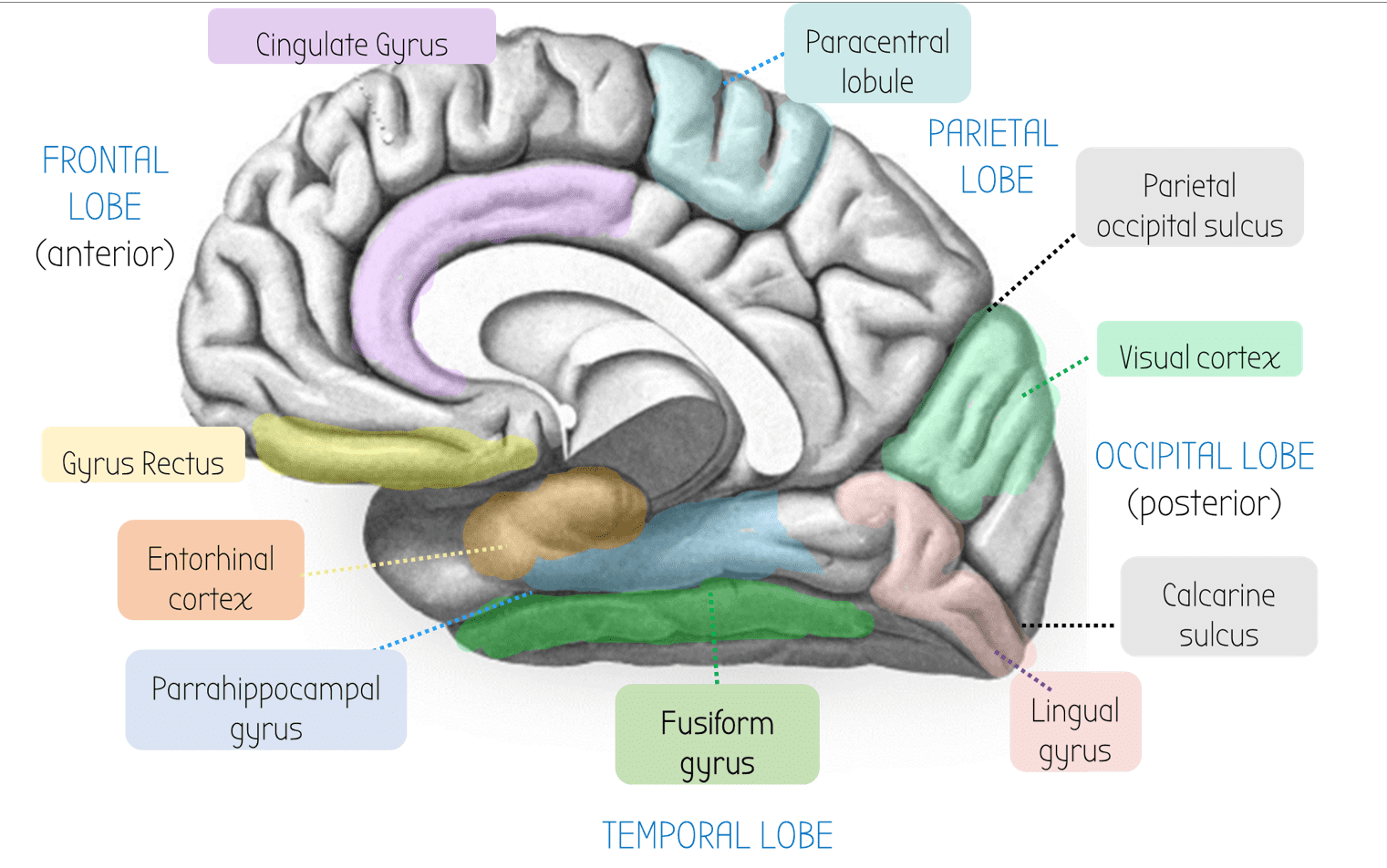
Paracentral lobule
🦵 Motor/somatosensory for leg
=Controls pee/poo 💩
--> Supplied by ACA = fecal/urinary incontinence 💩💩💩
Entorhinal Cortex
Part of the Parahippocampal gyrus - gateway to the hippocampus
Cingulate Gyrus
Contains large bundle of fibres called the cingulum. These run to the Parahippocampal gyrus, which connects to the hippocampus.
Frontal Cortex
Emotion and personality.
Parietal Occipital Sulcus
On the medial side of the cerebrum, this groove in the brain is the main thing that divides the parietal and the occipital lobe.
Gyrus Rectus
Responsible for taste
Fusiform Gyrus
Contains the fusiform face area (active in both hemispheres) which lets you recognise faces.
Lesions in the right fusiform face area FFA cause prosopagnosia - cannot recognise people's face
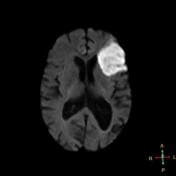
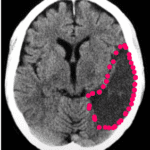
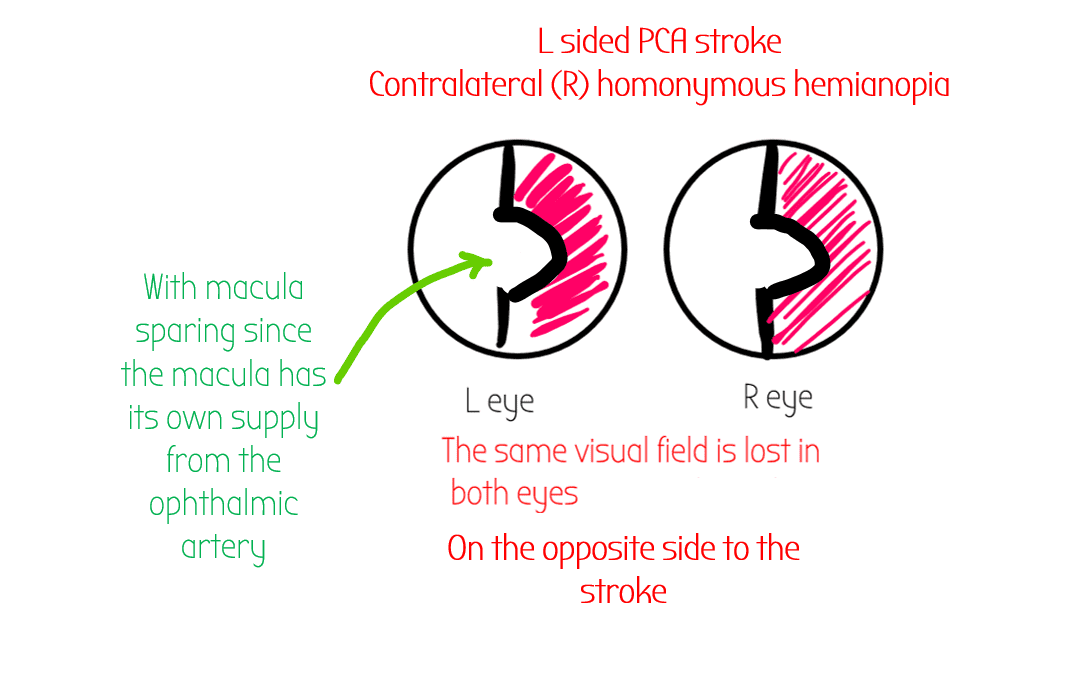
Visual Cortex
At the occipital lobe - supplied by the PCA
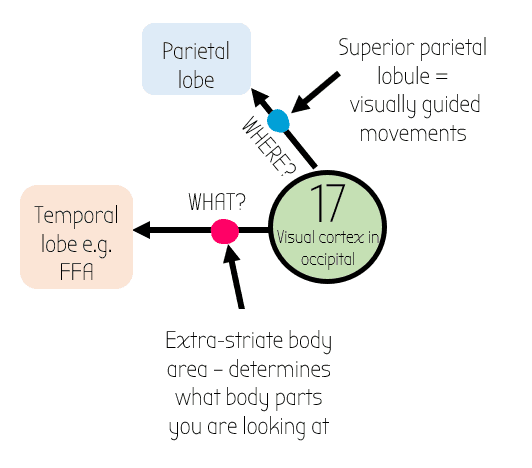
Visual Cortex AKA V1
Occipital lobe at the back – Brodmann area 17
Processes most of vision from the contralateral visual field
Connected to other parts of the brain
–> Goes up to parietal lobe for the WHERE? info
–> Goes across to temporal lobe for the WHAT lobe e.g. extrastriate body area & Fusiform Face Area
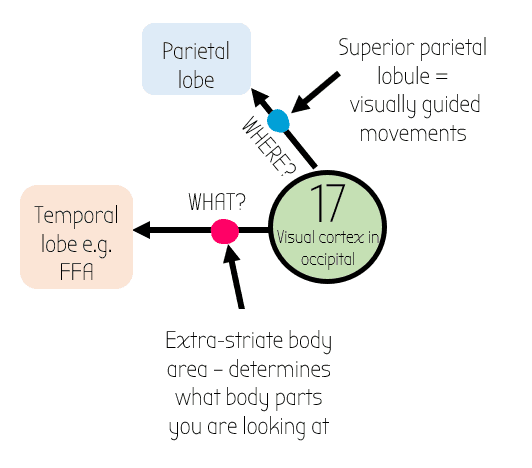
Receives info from reciprocal connections from Lateral Geniculate Nucleus LGN

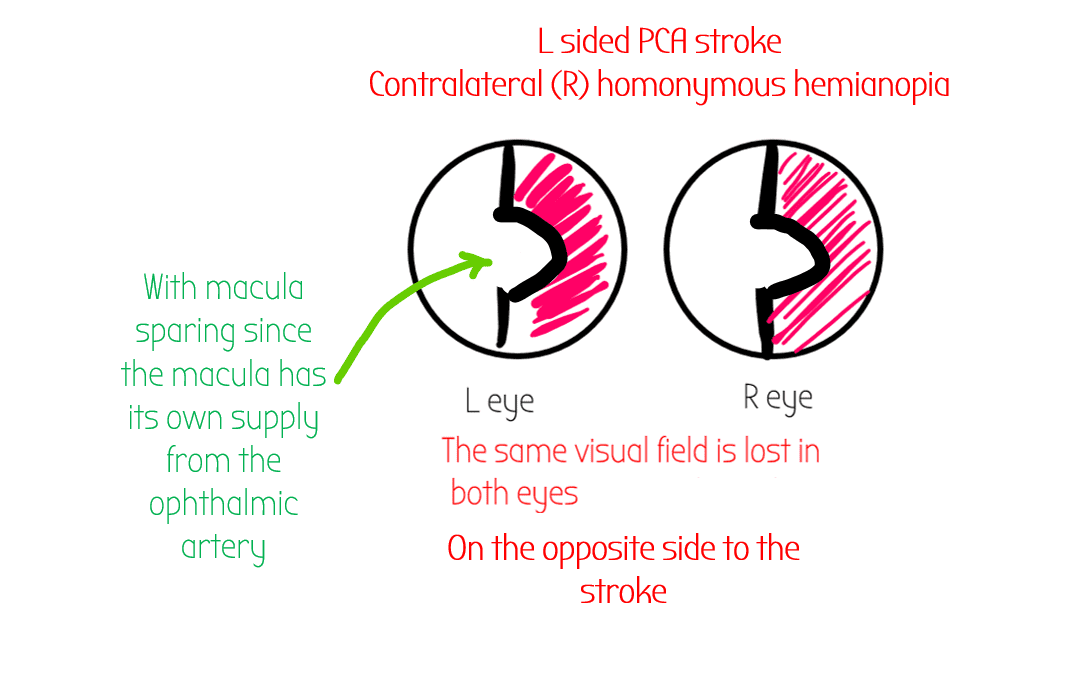
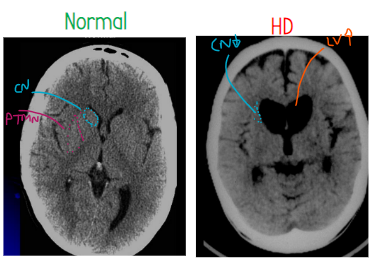
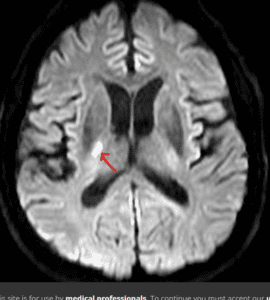
-PCA Stroke (below is a LEFT sided pca stroke – remember brain scans are always flipped)
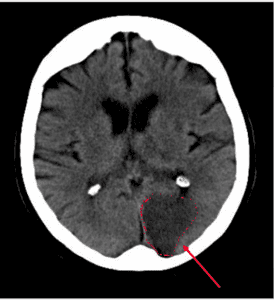
PCA stroke causes contralateral homonymous hemianopia (lost opposite to stroke half the visual field in both eyes ) WITH macular sparing
- Macula has its own supply from the ophthalmic artery (branch of ICA)
PCA stroke may also affect CNIII (oculomotor) – Weber’s Syndrome – Ipsilateral enlarged pupil and ptosis, down and out gaze – so recti don’t work and overpowered by SO & LR
Fusiform Gyrus
Medial temporal lobe
Conains fusiform face area FFA which recgonises people’s faces
Connected to V1 (area 17)

-PCA Stroke / lesion can cause problems in recognising faces – prosopagnosia
Basal Ganglia
The basal ganglia are a collection of neurones at the bottom of the brain that fine tune movement.
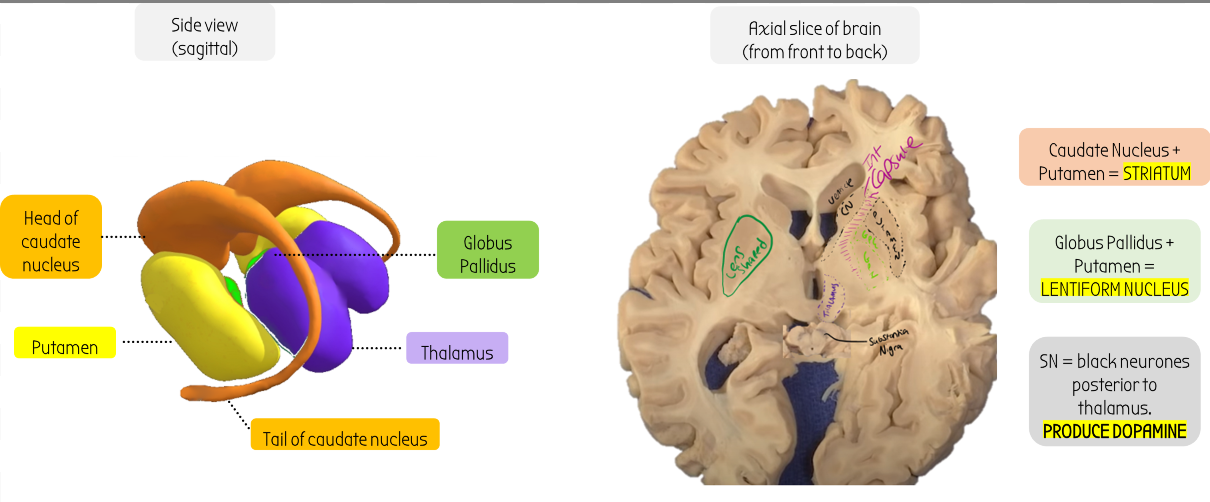
Putamen
The putamen makes up the striatum along with the caudate nucleus.
The putamen is deep to the INSULAR CORTEX (deep inside the lateral fissure)
Lentiform nucleus
Consists of GP + Putamen and makes a lens shape
Caudate Nucleus
Atrophies in Huntington's Disease HD
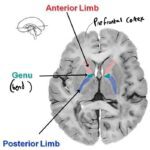
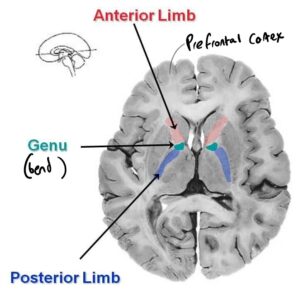
Internal Capsule
-not part of BG
-Posterior limb really important for movement
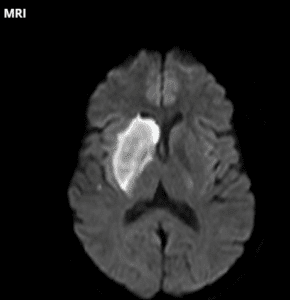
Axial MRI of Basal Ganglia
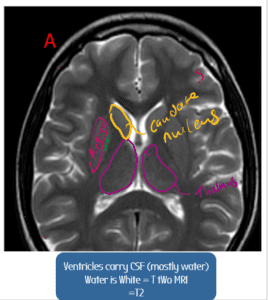
Lentiform nucleus
Consists of GP + Putamen and makes a lens shape
The basal ganglia has two pathways for movement - the direct and indirect pathways. These can be modulated by dopamine. See below:
Listen to the audio explanation here:
Listen to the audio explanation here:
Basal Ganglia Pathologies:
Pathology
Symptoms
Nuclei affected
Pathophysiology
Treatment
Parkinson's Disease
- Hypokinetic (low movement)
- Shuffling gait (hard to walk smoothly)
- Difficulty initiating movement
- Fingers moving at rest: pill rolling tremor (due to lack of fluid movement)
- Masked facial expressions
- Cogwheel rigidity: limbs/fingers move back and forth a bit like a cog turning
Degeneration of
Substantia Nigra – SN (produces dopamine)
- Dopamine leads to more movement in both pathways
- Often, mutations in the SNCA gene lead to the alpha-synuclein protein to misfold and become sticky
- These naughty proteins can aggregate into evil blobs called Lewy bodies
- Lewy bodies accumulate in SN & damage SN
- =LESS DOPAMINE PRODUCED
therefore lack of dopamine = less movement & problems initiating movement
-Direct pathway less active
-Indirect pathway more active

-e..g paramedian branch of basilar artery (causes Weber’s Syndrome)
contralateral parkinsonism (basal ganglia supply the motor area, then the fibres cross over)
As the problem is lack of dopamine, the main treatment is to give L-DOPA, a precursor to dopamine
- It is able to cross the Blood Brain Barrier (BBB)
Converted by DOPA decarboxylase from L-DOPA –> Dopamine
Side effects of dopamine (L-DOPA) therapy:




L-DOPA can act on peripheral dopamine receptors and cause nausea. There are two drugs (one works outside the brain – carbidopa, one inside the brain – domperidone) we can use to stop the effects of nausea:
- Carbidopa + benserazide (work outside brain) : inhibit peripheral breakdown of L-DOPA by dopamine DECARBOXYLASE. This means that less L-DOPA is needed to be delivered as less is wasted. As less is in the system, there is a lessened chance of side effects!
- Domperidone (works inside brain) – D2 receptor antagonist. The Chemoreceptor Trigger Zone (CTZ) is in the brainstem and dopamine acts on it to make you feel sick. Domperidone blocks this D2 activation of CTZ and therefore stops you from being sick.
Huntington's Disease
- Hyperkinetic jerky movements initially
- akinesia (lack of movement) later on
Sudden brief involuntary twitches all over the body
CN & Putamen
–CN (in blue) & Putamen (pink) atrophied
-Space filled by enlarged lateral ventricles (LV in orange)
Genetics:
- Mutations in the HD gene on the p arm of chromosome 4 (4p16.2) introduce more repeating sequences of ‘CAG’ glutamate codons (e..g CAGCAGCAGCAG etc)
- The excessive glutamate repeats (>40) cause the huntingtin protein to missfold and become sticky
- mutate huntingtin protein aggregates in the CN & putamen & causes them to atrophy
- Dominant inheritance & the disease shows genetic anticipation
Movement Pathways:
Remember, in both pathways, more dopamine = more movement.
The different stages of symptoms can be explained by different mechanisms:
- Initial chorea: jerky movements. (2 possible explanations)
- CAG repeats cause too much dopamine to be produced, leading to too much movement
- The indirect pathway degenerates first. The indirect pathway inhibits movement. Therefore by it degenerating, we get hyperkinetic movements
- Disease progresses to akinesia:
- Later on, the direct pathway degenerates.
- As both the direct & indirect are degenerated this leads to LACK OF MOVEMENT
Treatment
The hyperkinetic movements are thought to be due to excess dopamine release.
∴ DOPAMINE DEPLETION THERAPY
e.g. Tetrabenazine (dopamine antagonist – blocks dopamine from being packaged into vesicles by blocking the VMAT transporter)
Ballism
Symptoms
🦵 Large amplitude involuntary limb movements, especially lower lib (can affect just one leg – hemiballism)
Nuclei affected
Subthalamic nucleus
Pathophysiology
Subthalamic nucleus excites the yellow box.
IE the subthalamic nucleus makes the leash on the thalamus tighter, ie makes the thalamus more inhibited, therefore REDUCES MOVEMENT.
Destruction of the subthalamic nucleus can lead to excessive movement (hyerkinetic) aka ballism.
Treatment
N/A
Nuclei
Function
Pathologies
Striatum
(i.e. caudate nucleus + putamen)
Caudate nucleus + putamen = striatum
The striatum projects onto the Globus Pallidus via the direct and indirect pathways to control movement (see above)
The striatum also has D1 excitatory & D2 inhibitory receptors which respond to dopamine for the direct and indirect pathways. Overall, dopamine leads to more movement.
💊 The striatum has a nucleus in it called the nucleus accumbens which responds to cocaine and causes addiction! (don’t take coke all the time)
🩸Striatum is supplied by striate arteries (branch of MCA which comes from internal carortid) which also supplies the internal capsule. Ischaemia (blockage) in striate arteries = LACUNAR STROKE. Usually causes complete contralateral hemiparalysis (e.g. in this example, paralysis of the LEFT side of the body)
😟 Huntigton’s disease: hyperkinetic, jerky movements
-initially degeneration of indirect pathway (
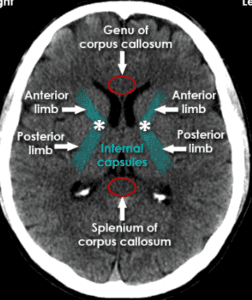
Internal Capsule
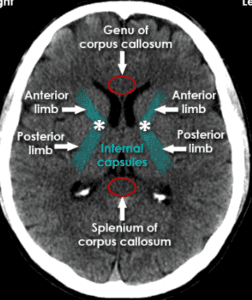
Not part of the basal ganglia but can be seen in the same cross sections.
A passage for fibres to pass through. The anterior bend (‘limb’) of the internal capusle contains the fibres for worrying about stuff.
The posterior limb contains fibres for movement of the contralateral side of the body
Posterior limb:
🩸Supplied by striate arteries that come from middle cerebral artery (which in turn come from internal carotid).
ALL descending contralateral motor neurons are found here.
These striate arteries also supply corpus-striatum, caudate nucleus & striatum
Stroke here (lacunar stroke) can lead to paralysis of the whole body!
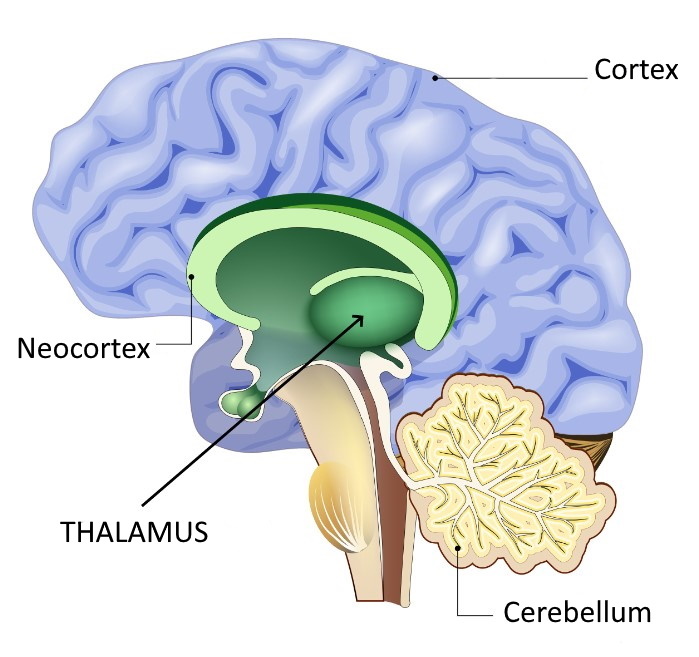
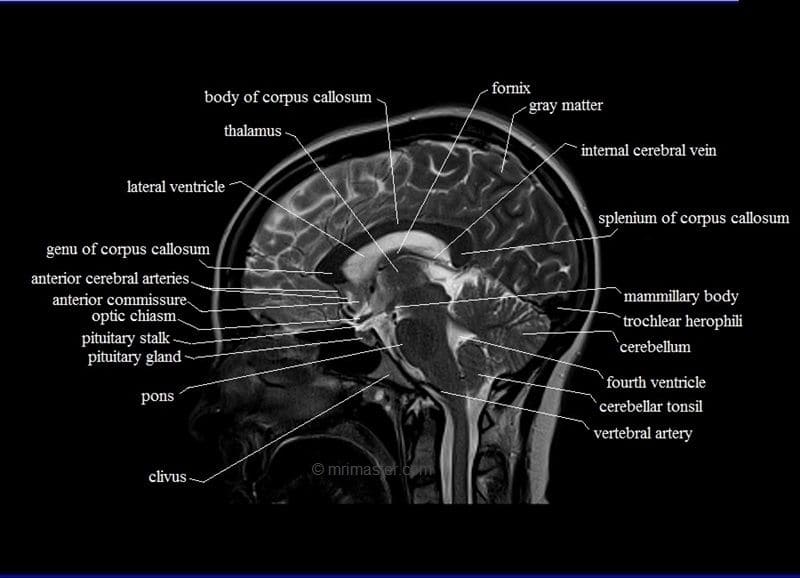
Thalamus
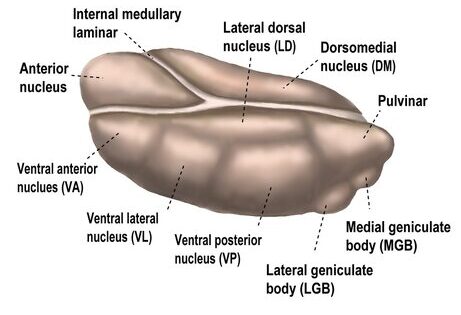
Lateral Geniculate Nucleus 👀
-> Connections to calcacrine vissue (v1)
--> Visual Processing
Anterior nucleus of thalamus
->Important for memory
--> Receives inputs from hippocampus via mammilo-thalamic tract
Medial Geniculate Nucleus 👂
-> Receives input from inferior colliculus blobby bit at the midbrain
--> Ouputs to primary auditory cortex in the lateral fissure of temporal lobe WITH A TONOTOPIC MAP
Pulvinar
Has connections with parietal lobe & some of occipital lobe
Ventral Anterior &
Ventral Lateral Nucleus
Motor processing
Outputs to supplementary motor area (SMA)
Dorsal medial nucleus of thalamus
Personality & Emotions
INPUT:
Amygdala
OUTPUT:
Prefrontal cortex - fibres pass through the anterior limb of internal capsule
Intralaminar nuclei
Receive information from reticular formations and give outputs to striatum + neocortex to keep you awake 😴
Ventral Posterior Nuclues of Thalamus
Somatosensory processing of the thalamus
VENTRAL POSTERIOMEDIAL 👅
- trigeminal nerve, face & tongue organisation
VENTRAL POSTERIOLATERAL 🧍 -
-whole rest of body --> major input to M1 motor cotex
Senses are processed here and sent off to other parts of the brain via reciprocal connections.
🤕 Damage to the thalamus (e.g. after a PCA stroke) can either stop you feeling pain contralaterally or cause SEVERE PAIN (severe pain = thalamic syndrome)
⚠️Absence Epilsepy Seizures (loss of awareness for a few seconds) involve thalamo-cortical circuits
Nuclei
Location
Function
Connections & Neurotransmitters
Lateral geniculate nucleus (LGN)
On the posterior of thalamus on the outside.
Visual processing.
Reciprocal connections to CALCARINE fissure (contralateral visual field info)
- Visual pathway comes from retina
- Crosses over at the optic chiasm (above the pituitary gland ) to the contralateral LGN
- This part of thalamus has reciprocal connectionswith area 17 (V1)
- Right geniculate nucleus connects with right side of primary visual cortex
- Primary visual cortex – calcarine sulcus
Medial geniculate nucleus
On the posterior of thalamus on the inside
Auditory processing
- Inner ear – cochlear part of VIII (8th) nerve goes to cochlear nuclei in brainstem & synapses in inferior colliculus in midbrain
- medial geniculate nucleus in thalamus –> primary auditory cortex in cerebrum (buried in lateral fissure on superior surface of temporal lobe)
- There is a tonotopic map – each part of the cortex responds to different frequency
Ventral posterior VP nucleus
Nucleus at the very posterior of the thalamus on the lateral side (outside bit)
Somatosensory nucleus of the thalamus – sensory processing.
Maintains a somatotopic map (remembers where the sensation originated from 😮)
VENTRAL POSTERIOMEDIAL – trigeminal nerve, face & tongue organisation
VENTRAL POSTERIOLATERAL – whole rest of body –> major input to M1 motor cortex
INPUTS:
- Medial lemniscus (point discrimination, vibration sense, conscious) proprioception)
- Spinothalamic tract (pain, temp, light, touch)
- Info goes to somatosensory areas (S1 in parietal lobe) in the brain
- Ventral posteriolateral is a major input to the M1 motor cortex
Damage to the thalamus (e.g. after a PCA stroke) can either stop you feeling pain contralaterally or cause SEVERE PAIN (severe pain = thalamic syndrome)
Ventral lateral nucleus
Closer to the front of the thalamus, on the outside (lateral)
Motor processing
- INPUT: Purkinje cell of pontocerebellum (lateral cerebellar hemispheres)
- OUTPUT: Ventral posteriolateral is the major input to the M1 motor cortex
Ventral anterior nucleus
At the very front of the thalamus
Motor processing
INPUT:
- Receives info globus pallidus (basal ganglia)
- & Dentate nucleus (cerebellum)
OUTPUT:
- Basal ganglia –> Supplementary motor area (area 6)
Dorsomedial nucleus of thalamus
Medial bit of thalamus
Emotion
- Receive info from amygdala (emotion)
- Output fibres go through the anterior limb of the internal capsule, to the prefrontal cortex (front bit of the brain, controls emotions)
Interlaminar nuclei
Nucleus inside the thalamus, underneath the internal medullary laminar
Receive information about nociception from reticular formation & keep you awake
- Receive info from reticular formations
- Activates striatum (basal ganglia) + neocortex to keep you awake
- Damage to the reticular formation in the brainstem (e.g. locus cereleus) can damage this system and put you into a coma. Deep brain stimulation of these areas may help to wake you up again 🙂
Hypothalamus & Limbic System
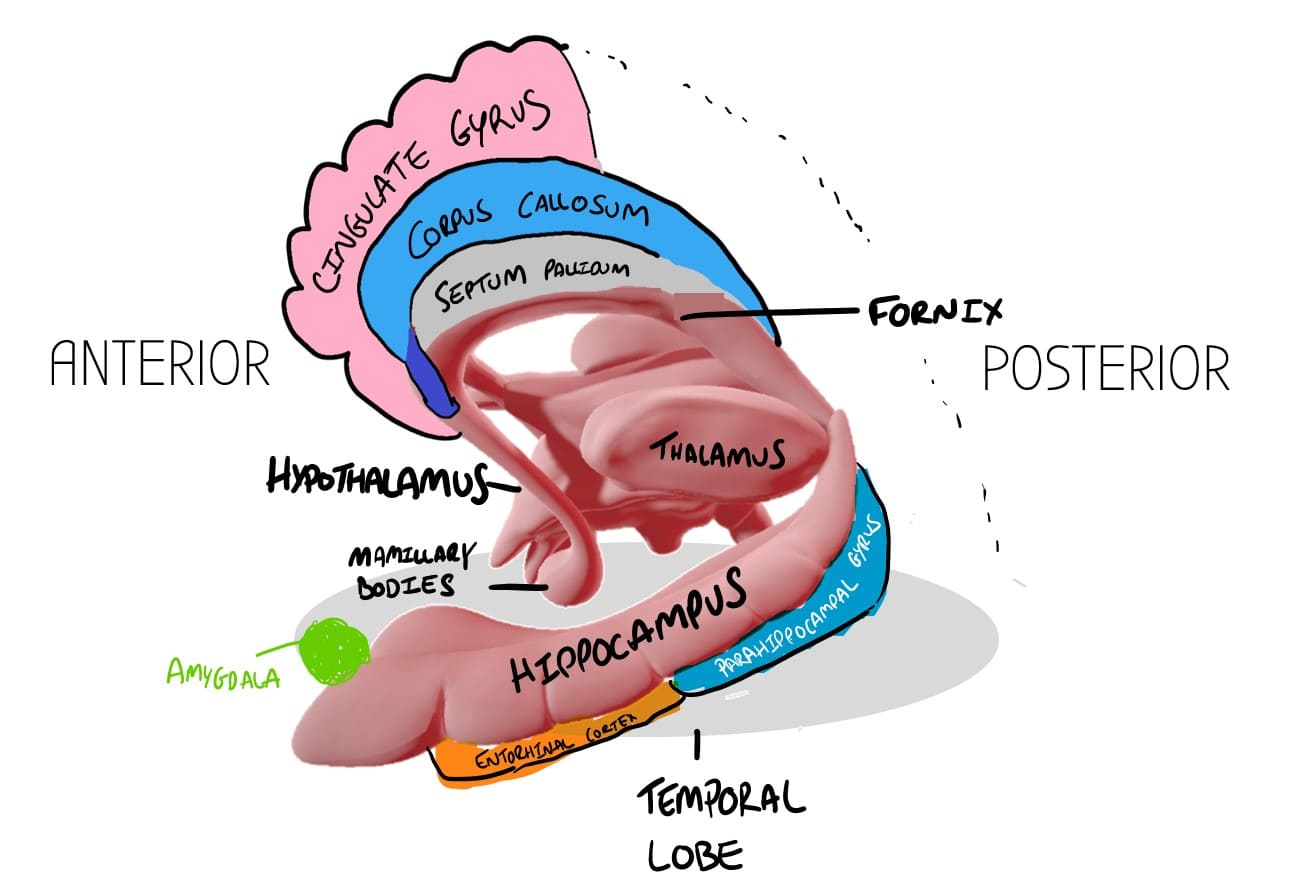
Cingulate Gyrus
Contains large bundles of axons called the cingulum. These run to the Parahippocampal gyrus, and then connect to the hippocampus via the entorhinal cortex.
Corpus Callosum
Connects the two hemispheres of the brain together.
ACA follows around the corpus callosum.
Septum Pellucidum
Makes up the base of the lateral ventricles. There are four ventricles in the brain, two in each hemisphere, a third one that joins them together in the middle, and the 4th ventricle which drains into the cerebral aqueduct which connects to the spinal cord. 
Ventricles drain CSF around the brain
Anterior Commisure
Bit of white matter that connects both hemispheres.
Its close to the nose - olfactory processing/smell occurs here.
Mamillary Body

At the anterior end of the fornix, where it joins onto the hypothalamus, there are two bulbs which make up the mamillary bodies.
Function: Recollective Memory
🍷 Damaged by alcohol causing problems in memory: Korsakoff's syndrome 🙁
Thalamus
Not part of the limbic system but sits on top of hypothalamus (below the thalamus!)
Thalamus has reciprocal connections to the rest of the brain - receives inputs e.g. from eyes/ears/ cerebellum and then outputs to other movement/sensory areas in the cortex
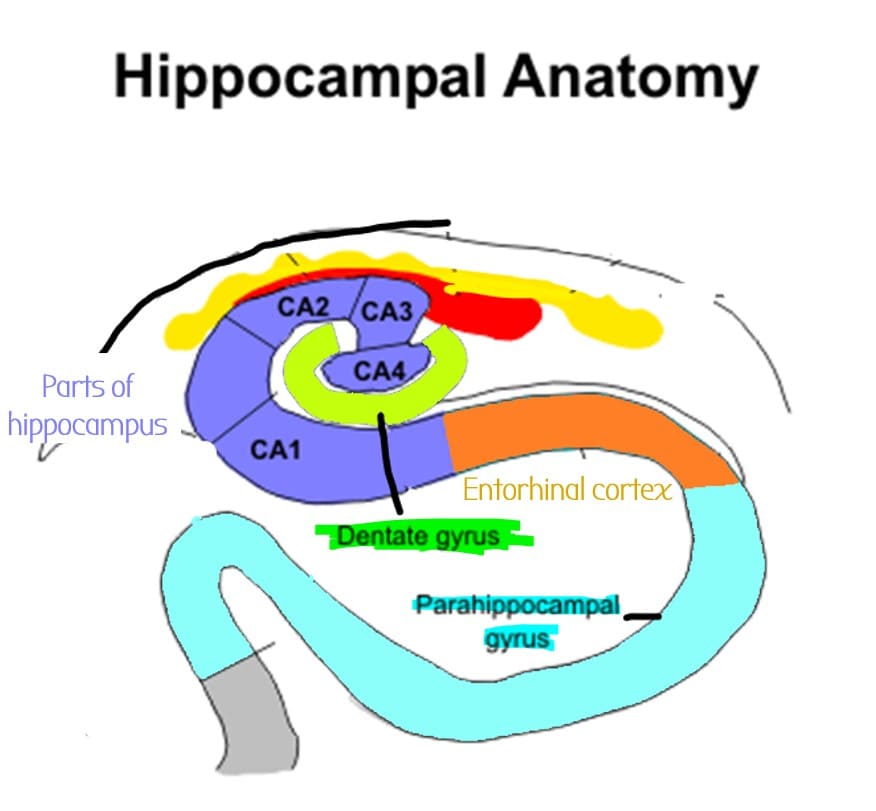
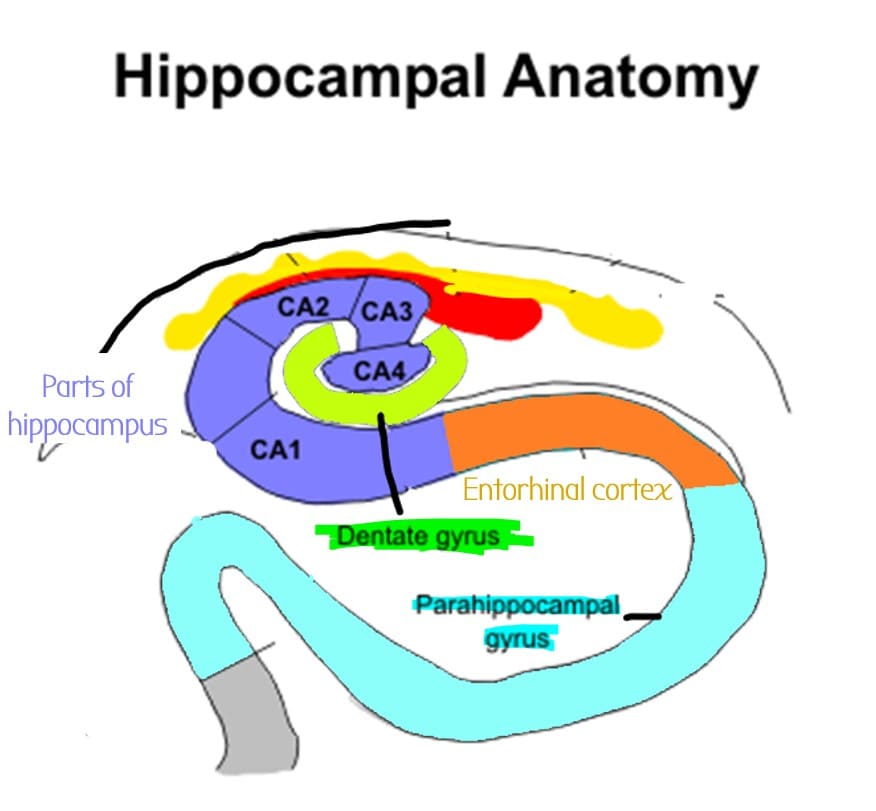
Entorhinal cortex
Part of the parahippocampal gyrus, Gateway for information into/ out of hippocampus
Sits underneath hippocampus
- Info about memories comes from here enters the hippocampus through the DENTATE GYRUS
- Then goes to CA3 part of hippocampus
Amygdala
Important for emotional regulation (e.g. the emotional response to pain 😥 )
► Amygdala removed (e.g. if the anterior temporal lobe is removed) = kluver-bucy syndrome - memory loss, hypersexuality 🍆🍆, visual agnosia
Hippocampus 🦛
⚠️ If Hippocampus is involved in focal seizures, you get Deja-vu
Medial Temporal Lobe
The hippocampus is super important for episodic memory (memories about events) and it sits in the medial temporal lobe.
🦠 Medial temporal lobe is prone to bacterial/viral infections/ meningitis which can damage it and therefore cause memory loss 🙁 🦠
Parahippocampal gyrus
The gyrus next to the hippocampus
Continous with the cingulate gyrus
📍 Has a PLACE AREA - important for recognising places
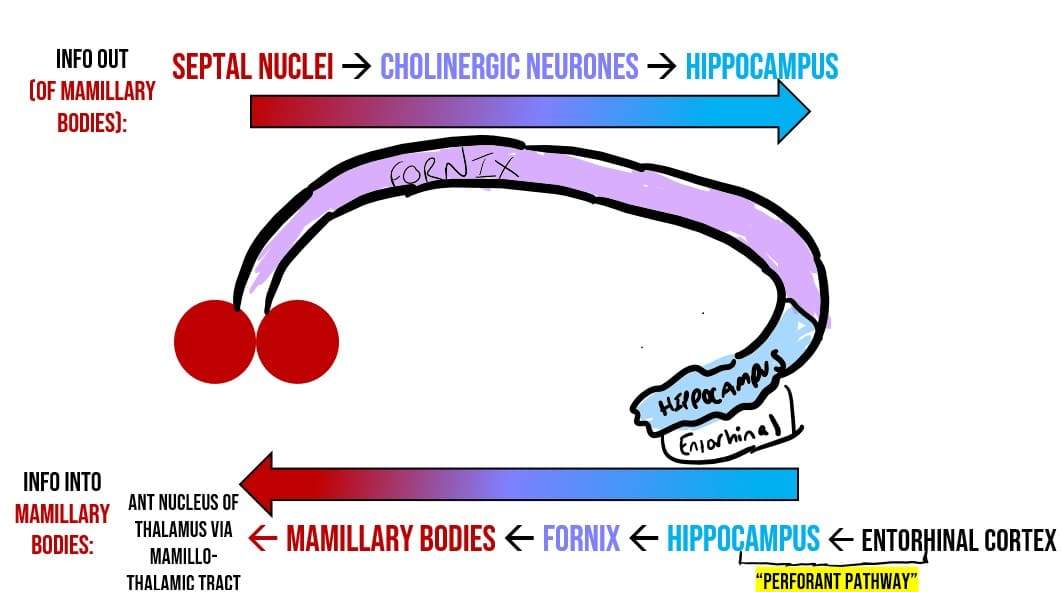
Fornix
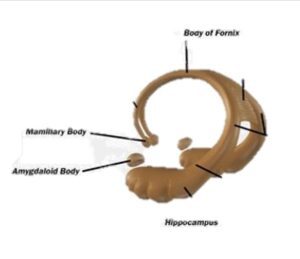
Tract of white matter that carries info into and out of hippocampus 🦛
It ends in two bulbs - the mamillary bodies which are part of the hypothalamus.
Fornix carries info out of hippocampus into the mamillary bodies
& Out of the septal nuclei in the mamillary bodies into the hippocampus.
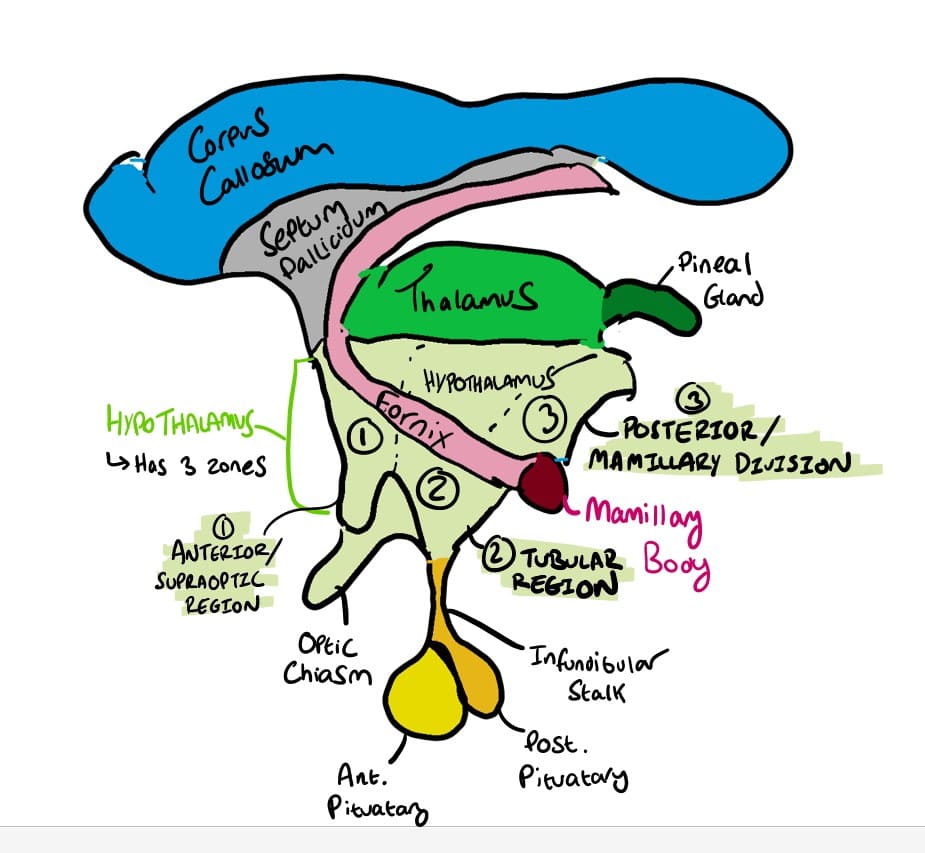
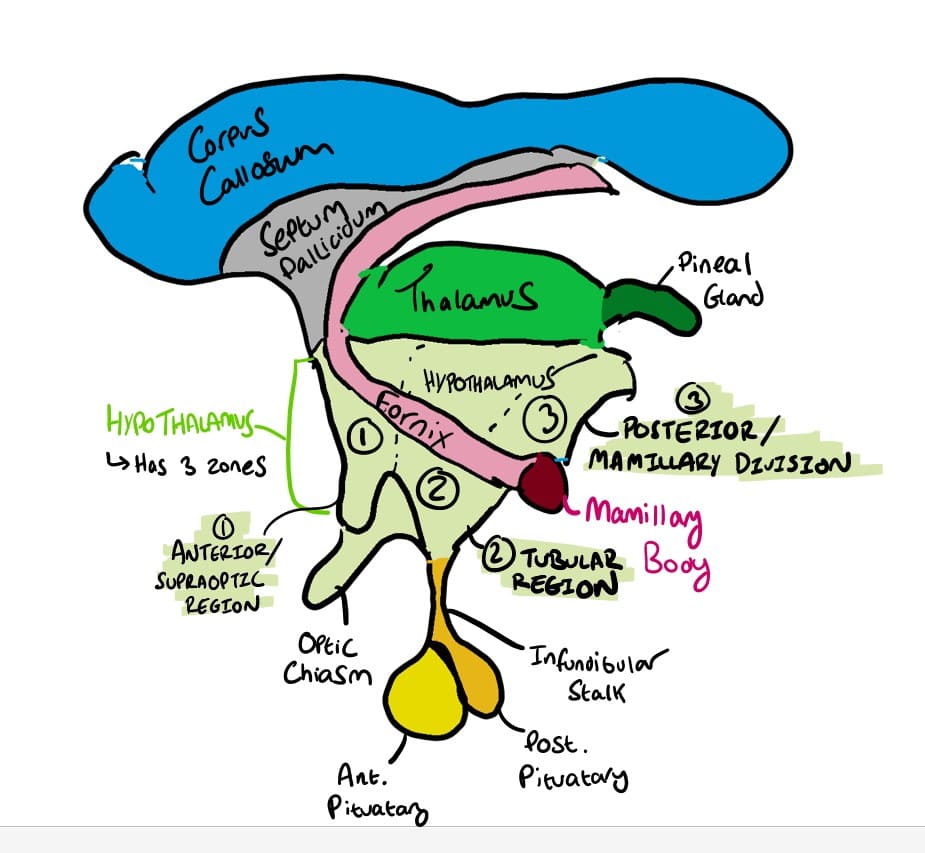
Hypothalamus
- Sits underneath thalamus
- Important for homeostasis
- Has three regions:
The limbic system is made of the hippocampus, parahippocambpal gyrus, hypothalamus, amygdala & fornix. It is responsible for emotion, behaviour and memory
Mammillary Bodies
Two bulbs at the end of the fornix. Gateway to the hypothalamus
Info flows to/from hippocampus into & out of the mamillary bodies via the fornix.
The fornix is a tract of white matter that carries info between these two.
Mamillary bodies are also important in memory.
🍷🍷 In alcoholics, malabsorption of B1 –> mammillary bodies shrivels , can lead to amnesia and confabulation (making up memories to fill the gaps) – AKA WERNICKE- KORSAKOFF SYNDROME
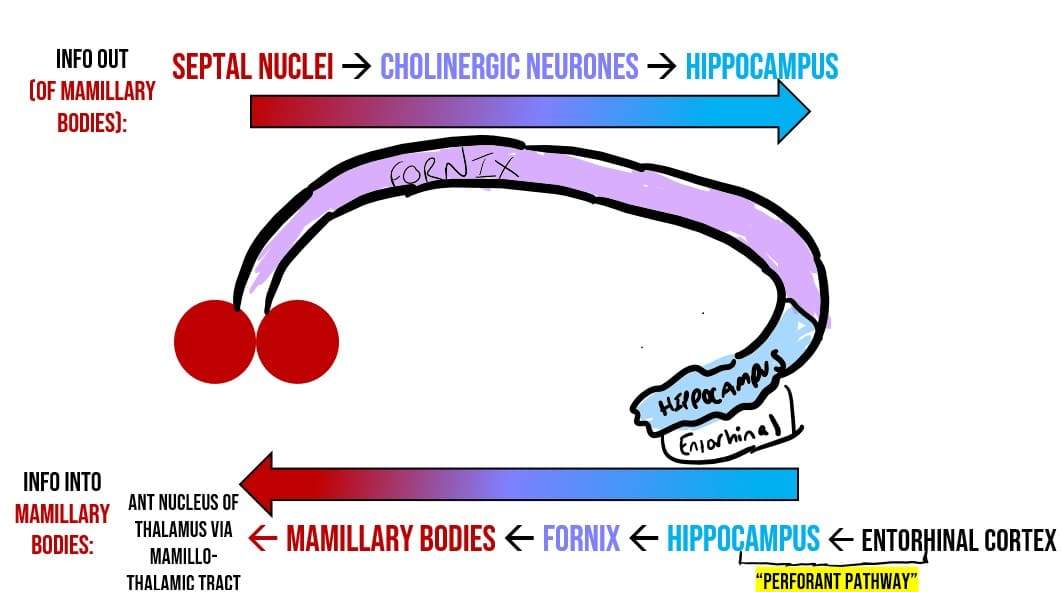
Hippocampus
Two bulbs at the end of the fornix. Gateway to the hypothalamus
Memory formation.
- Damage to medial temporal lobe can lead to loss of episodic memory (patient HM)
Contains regions CA1, CA2, CA3, & the dentate gyrus
Contain special neurones for spatial stuff:
- place cells – where something is
- Grid cells – which direction something is moving
Info can enter hippocampus through:
- Perforant pathway
- Septohippocampal cholinergic neurones
Info out of hippocampus leaves via the fornix, goes to the mamillary bodies –> anterior nucleus of thalamus
Alzheimer’s disease: misfolded evil Tau proteins can spread from entorhinal cortex, through the hippocampus, then through the temporal lobe and then the neocortex
⚠️ If Hippocampus is involved in focal seizures, you get Deja-vu
Hypothalamus
Sits below (hypo) the thymus.
Important for homeostasis.
Divided into three zones:
- supraoptic region,
- tubular region,
- mamillary region (the numbers are only for this diagram)
Because the hypothalamus is so close to the pituitary gland, it is able to control the release of hormones. For example, it produces GnRH – which causes the release of LH/FSH.
Nuclei/ Regions
Contains
Function
1
Supraoptic Region
Contains:
-Paraventricular Nuclei PVN
-Supraoptic Nuclei
PRODUCE ADH/OXYTOCIN THAT GOES TO POSTERIOR PIUTATARY GLAND AND THEN TO CIRCULATION
PVN:
Important for autonomic regulation. (ESR link)
- Synthesises ADH & Oxytocin (made by magnocellular neurones)
- The ADH is packaged into granules with neurophysin
- Enters the bloodstream (inferior hypophyseal circulation) via the supraoptic hypothalamic tract
- ADH makes your wee more concentrated (more ADH when you are thirsty)
🐣🐣🐣 When giving birth, contractions activate stretch receptors- This has positive feedback on the neurosecretary cells in the hypothalamus
- More OXYTOCIN IS RELEASED
- Targets the myometrium making the contractions even more forceful = 👶
2
Tubular Region
////////
Makes up the tubular-infiundibulary region
Just above the stalk of the pituitary gland (infundibular stalk)
Contains:
-Arcuate Nucleus
-Tubular Mamillary Nucleus (because it is next to the mamillary bodies of the fornix)
HUNGRY/SLEEPY CONTROL ZONE
ARCUATE NUCLEUS:
- Controls Appetite by having leptin receptors (adipocytes release leptin to make you feel full/satiated)
- Fibres cross at midline here
- Also produces dopamine which acts to inhibit the release of prolactin (lactating hormone
) AKA DOMINANT NEGATIVE CONTROL
- ie Prolactin is basically always switched off (by dopamine) unless you are pregnant
- Therefore anti-psychotics that block D2 dopamine receptors (e.g. Risperidone, apomorphine) also stop arcuate nucleus from producing dopamine = lead to the side effect of high prolactin
- =hyperprolactinaemia! (can cause unwanted lactation)
TUBULAR MAMMILARY NUCLEUS:
- Tubular mamillary nucleus controls wakefullness.
- The only histamine nucleus in CNS.
- Therefore antihistamines can make you sleepy
- Area damaged in ENCEPHALITIS LETHARGICA – sleeping for upto 20hrs a day!
- The interlaminar nuclei of the thalamus also control sleepiness
3
Posterior/
Mammillary Region
Contains Mamillary Nuclei
TEMPERATURE ZONE
- Mamillary nuclei = memory & thermoregulation
- Lesions here can cause HYPOthermia (hypothalamus –> hypothermia).
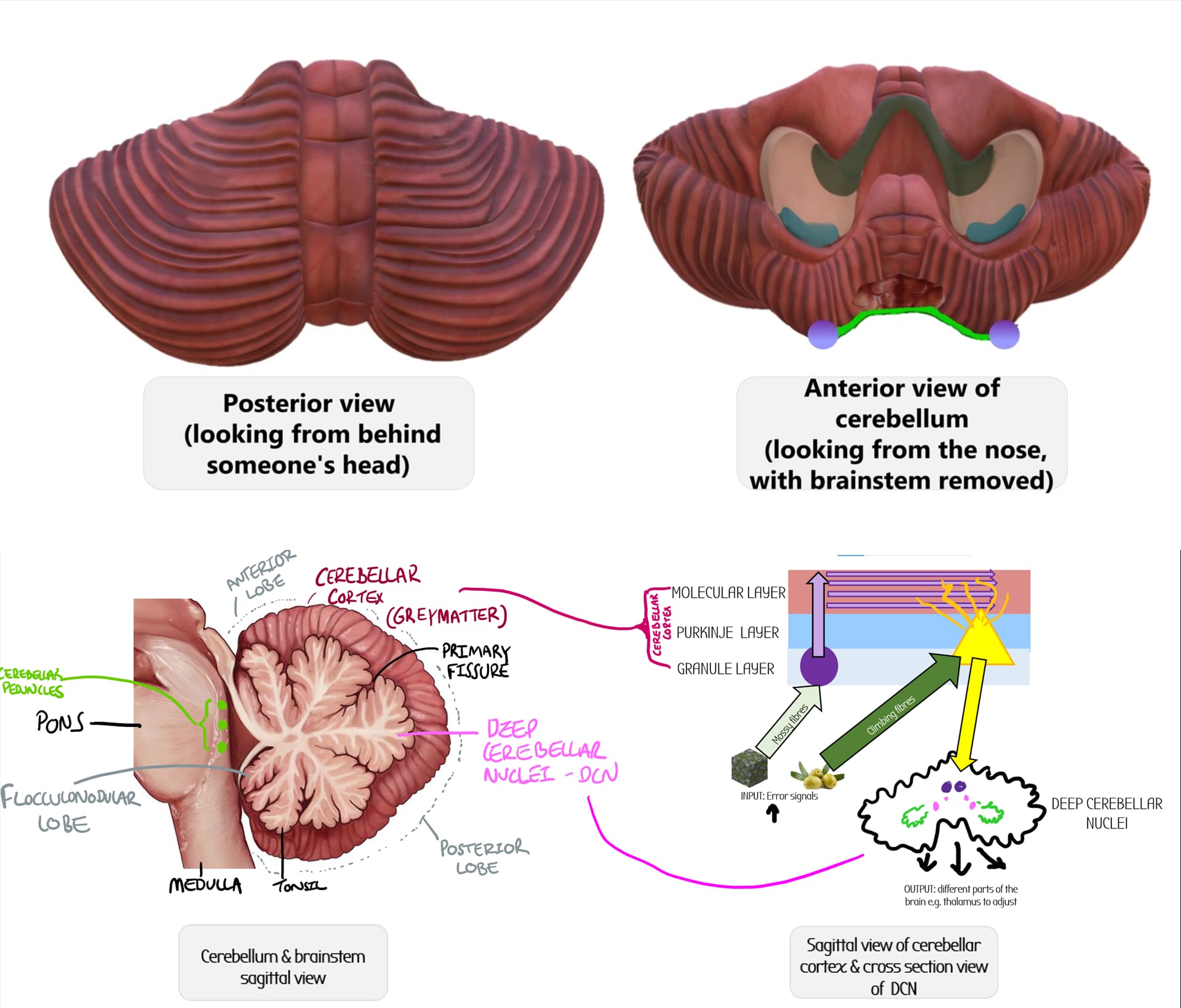
Cerebellum
The cerebellum is the mini-motor brain that sits at the very back of the brain, posterior to the brainstem.
It is responsible for fine tuning of motor movements, and receives inputs such as proprioception & error signals, and outputs via the DCN to different motor areas.
Cerebellar lesions/strokes lead to DANISH:
- Dysdiadochokinesia (inability to rapidly pronate/supinate hand)
- Ataxia (gait and posture)
- Nystagmus (eye muscle movements)
- Intention tremor
- Speech problems
- Hypotonia (decreased muscle tone)
Vermis
Long worm thing that runs along the middle of the cerebellum, and separates the left and right hemispheres
Primary Fissure
Separates the anterior and the posterior lobes of the cerebellum
Anterior Lobe
-Consists of parts I-V (1-5) of the cerebellum
-Lesions in the anterior lobe lead to GAIT ATAXIA .
- The anterior lobe of the cerebellum can be damaged in alcoholics (in Korsakoff's syndrome)
- Alcohol = malabsoprtion of Vit B1 = brain damage e.g. anterior lobe of cerebellum
Posterior Lobe
-Consists of parts VI-IX (6-9) of the cerebellum
Superior cerebellar peduncle
-connects to pons
Middle cerebellar peduncle
-Biggest peduncle
- connects to pons
Inferior cerebellar peduncle
- connects to pons/open medulla
- Dorsospinal cerebellar tract enters cerebellum from here (proprioceptive)
Spinocerebellum
Along the vermis & intermediate zones
Receives info about proprioception
Function:
- Receive a lot of information from spinocerebellar tracts (e.g. conscious proprioception, discriminative touch, temperature, pain etc)
- Controls dorsolateral descending systems (rubrospinal and corticospinal)
- Adjust ongoing movement of whole body .
Anterior lobe vermis particularly sensitive to alcohol misuse. Lesions here can cause ataxia of gait
Lateral Lobes: pontocerebellum
Function:
Assist in fine movement control:
Influences motor (M1) and premotor (area 6) cortex via VENTROLATERAL NUCLES OF THALAMUS
SEND INFORMATION TO THE DENTATE NUCLEUS
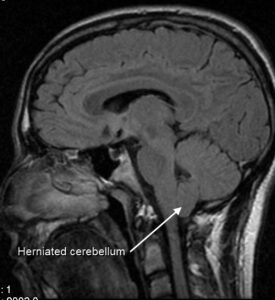
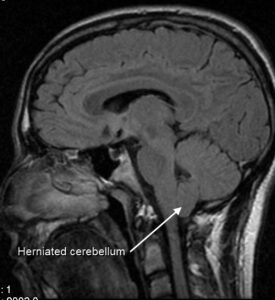
Cerebellar tonsil
Just above the floccular-nodular lobe there are two bumps at the lower surface of the cerebellm called the cerebellar tonsil.
These can herniate into the foramen magnum, and compress the medulla of the brainstem - breathing difficulties (chiari malformation).
Flocculus (part of the floccular-nodular lobe)
Anatomy:
-Part X (10) of the cerebellum
-At the very bottom of the cerebellum, visible from the inferior surface (you can barely see it from this view)
-The posterior lateral fissure divides the posterior lobes from the flocular-nodular lobes.
Function: Vestibulocerebellum
Controls balance & eye movement (eyes & ears!)
Damage = deficits in visual tracking , nystagmus (oscillation of eye movements), vestibulo-ocular reflex errors and balance problems
Cerebellar tonsil
Just above the floccular-nodular lobe there are two bumps at the lower surface of the cerebellm called the cerebellar tonsil.
These can herniate into the foramen magnum, and compress the medulla of the brainstem - breathing difficulties (chiari malformation).
Floccular-nodular lobe
Anatomy:
-Part X (10) of the cerebellum
-The posterior lateral fissure divides the posterior lobes from the flocular-nodular lobes.
Function: Vestibulocerebellum
Controls balance & eye movement (eyes & ears!)
Damage = deficits in visual tracking , nystagmus (oscillation of eye movements), vestibulo-ocular reflex errors and balance problems
Choroid plexus of 4th ventricle
Produces CSF
Cerebelllar peduncles
Three masses of tissue that connect pons to the cerebellum.
Can be seen in cross section e.g. here:
Primary Fissure
Landmark that separates anterior from posterior lobes
Anterior Lobe
-Consists of parts I-V (1-5) of the cerebellum
-Lesions in the anterior lobe lead to GAIT ATAXIA .
- The anterior lobe of the cerebellum can be damaged in alcoholics (in Korsakoff's syndrome)
- Alcohol = malabsoprtion of Vit B1 = brain damage e.g. anterior lobe of cerebellum
Cerebellar cortex
The outer bit of the cerebellum is the cerebellar cortex which is folded into folia
It is the external grey matter layer (cell bodies) and consists of three layers:
- molecular layer
- Purkinje layer
- Granule layer
input fibres come in at these layers and then exit via purkinje cells to the deep cerebellar nuclei
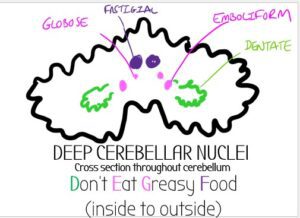
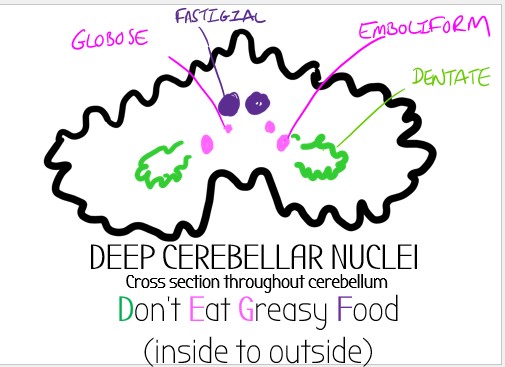
DCN
- 4 nuclei (dentate, emboliform & globose, fastigial)
- The cerebellar cortex projects to here via purkinje cells.
- These then go onto project to other parts of the brain
Mossy Fibres
- Contain proprioceptive information
- There are two sources of mossy fibres (from the pons & from the spino cerebellar tract)
- They enter at the granule layer and connect to granule cells. These granule cells go up and turn into millions of parallel fibres
- The parallel fibres connect onto purkinje cells, the output cells of the cerebellar cortex and then go to the deep cerebellar nuclear (DCN)
Parallel fibres
- Non-concious proprioception information (e..g where your body parts are without you thinking about it) -->
- Spinocerebellar tracts
- --> Mossy fibers
- --> Granule cells
- --> 250,000 Parallel fibers in the molecular layer of cerebellar cortex
- --> Purkinje cell (receives lots of parallel fibres but only has one output fibre!)
- DCN to be processed!
Climbing fibres
Contain error signals
Come from contralateral inferior olive of medulla - remember olive trees climbs
Go directly to the output cells (purkinje), without going through parallel fibres
Each purkinje cell only receives one fibre
(The climbing fibres themselves can project to several purkinje cells)
- From here they go to the DCN
Mossy Fibres
- Carry Error Signals to the cerebellum
- SOURCES:
- Pons –> Middle Cerebellar Peduncle (e.g. vestibular 👂)
- Dorsospinal Cerebellar Tract –> Inferior Cerebellar Peduncle (proprioception 👋 )
- ROUTE:
- Fibres arise from either middle/inferior cerebellar peduncle then:
- Go into granule layer of the cerebellar cortex
- Connect to granule cell
- Granule Cell projects the mossy fibres upwards into the molecular layer of cerebellar cortex
- From here, the mossy fibres become lots of fibres running parallel to each other (parallel fibres)
- Connect with purkinje cells to output
- PURKINJE CELL OUTPUT
- LOTS of parallel fibres connect to ONE purkinje cell
- Purkinje cell has one output fibre to the deep cerebellar nuclei to make adjustments
Climbing Fibres
- Carry Error Signals to the cerebellum e.g. retinal slip
- SOURCES:
- ALL ARISE FROM THE INFERIOR OLIVE
- Olive trees climb!
- ALL ARISE FROM THE INFERIOR OLIVE
- ROUTE:
- Fibres come from the inferior olivary nuclei in the olives in the medulla
- Cross the midline (CONTRALATERAL) and go to inferior cerebellar peduncle
- From here, they form climbing fibres
- These climb directly to the purkinje cell (without splitting into parallel fibres)
- PURKINJE CELL OUTPUT
- ONE CLIMBING FIBRE TO ONE PURKINJE CELL (1:1)
- Purkinje cell has one output fibre to the deep cerebellar nuclei to make adjustments
Nuclei/ Cerebellum landmark
Location
Function
Connections & Neurotransmitters
Anterior Lobe
The top bit of the cerebellum
Parts I-V (1-5) of cerebellum
Problems here lead to GAIT ATAXIA
- The anterior lobe of the cerebellum can be damaged in alcoholics (in Korsakoff’s syndrome)
- Alcohol = malabsoprtion of Vit B1 = brain damage e.g. anterior lobe of cerebellum
Vermis
Thing that runs along the middle of the cerebellum (separates left/right hemispheres)
Spinocerebellum
Receives info about non-conscious proprioception (that you don’t consciously think about)
- Receive a lot of information from spinocerebellar tracts (e.g. conscious proprioception, discriminative touch, temperature, pain etc) .
Anterior lobe vermis particularly sensitive to alcohol misuse. Lesions here can cause ataxia of gait
INPUT: Spinocerebellar tracts
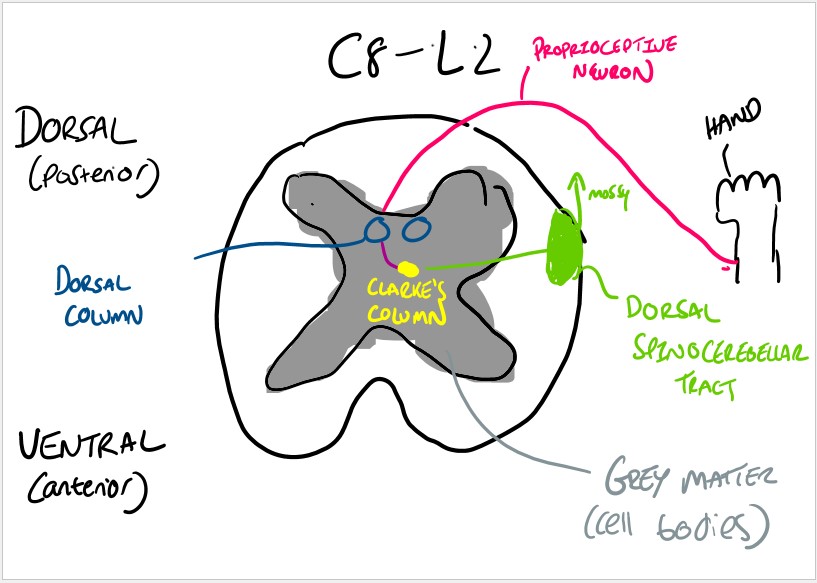
- These tracts contain proprioceptive info
- Info comes from proprioceptive neurones, which go to the dorsal column, synapse at Clarke’s column in the grey matter (Cell bodies)
- This neuron then goes to the white matter (tracts) and travels up the dorsal spinocerebellar tract
- The tract goes to the inferior cerebellar peduncle –> vermis
- Fibres becomes mossy fibres, then parallel fibres
- Project onto one purkinje cell –> Globose/Emboliform nuclei
OUTPUT:
- Controls dorsolateral descending systems (rubrospinal and corticospinal)
Lateral Lobes of cerebellum
Left/Right side of the cerebellum
Make up the pontocerebellum (fine movement)
OUTPUT:
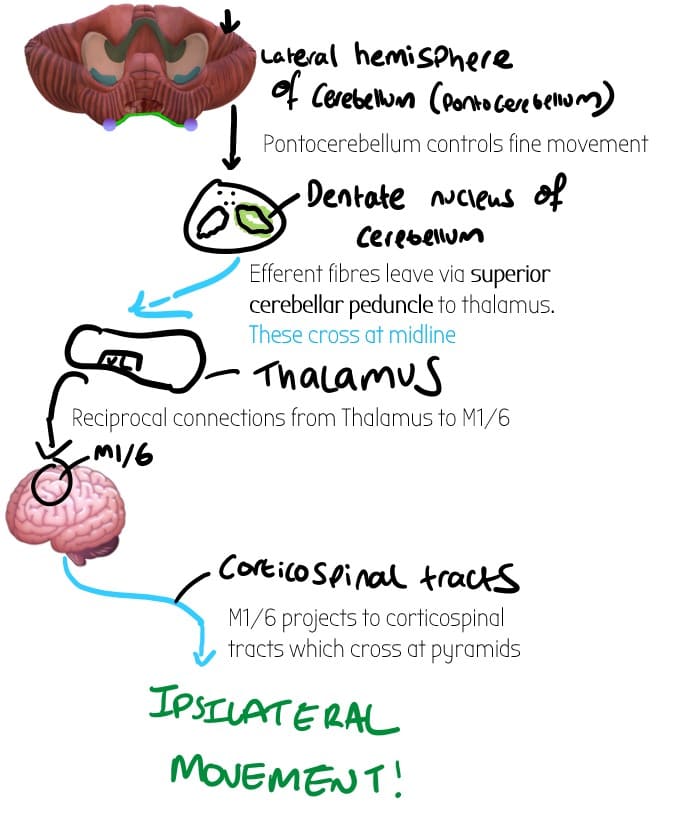
- Outputs information about planning movements to the Dentate Nucleus
- Dentate nucleus has efferent projections (outputs) which leave via the SUPERIOR CEREBELLAR PEDUNCLE
- These go to the ventrolateral nucleus of thalamus & crosses the midline
- The ventrolateral nucleus of the thalamus projects to the motor (M1) and premotor (area 6) cortex in the cerebrum
- The cerebrum sends these motor signals out via corticospinal tracts which cross at the pyramids
- Because there is double crossing, the cerebellum has ipsilateral motor control
Floccular-nodular Lobe of Cerebellum
Part X of cerebellum – at the inferior surface
Makes up the vestibulocerebellum (along with a small part of the vermis)
Receives input from the vestibular labyrinth (three loops in the ear filled with endolymph and the utricle and saccule) , and projects directly to vestibular nuclei .
-Controls balance & Eye movements
Damage = deficits in visual tracking , nystagmus (oscillation of eye movements), vestibulo ocular reflex errors and balance problems
The vestibulocerbellum receives error signals from the eyes and ears:
floccular-nodular lobe
-👂 semi-circular canals in ears filled with endolymph. Balance error signals carried by CN VIII into mossy/parallel fibres:
Small part of vermis
-👀 error signals about retinal slip (eye movement) via pretectal nucleus –> inferior olive —> Climbing fibres
-Vermis also receives input from neck and trunk
From here, the error signals (mossy/climbing fibres) project onto Purkinje fibres which then output the error information to the FASTIGIAL NUCLEUS
After going to the fastigial nucleus, the purkinje axons then leave the cerebellum:
floccular-nodular lobe
Project directly to
- vestibular nuclei in the dorsolateral medulla (supplied by PICA)
- Reticular formation
Small part of vermis
Output through reticulospinal, vestibulospinal and corticospinal fibres through the inferior cerebellar peduncle
Superior cerebellar peduncle
The most superior peduncle of the cerebellum, near choroid plexus of 4th ventricle
The cerebellar peduncles are masses of tissue that connect the brainstem (pons) to the cerebellum
OUTPUT (efferents):
-lateral hemispheres of the cerebellum (pontocerebellum) control fine movement
-These fibres exit the cerebellum and cross at the superior cerebellar peduncle (contralateral)
- Gives small input to red nucleus (midbrain)
- Gives larger input to thalamus and onto motor cortex (ventrolateral thalamus –> M1 – precentral gyrus & ventroanterior thalamus –> area 6 premotor cortex PMC)
- Also project to reticular formation in brainstem
Middle Cerebellar Peduncle
At the level of the pons.
The biggest of the three cerebellar peduncles.
The cerebellar peduncles are masses of tissue that connect the brainstem (pons) to the cerebellum
SOURCE OF MOST MOSSY FIBRES
The biggest cerebellar peduncle that connects the pons to the medulla
Because it is the biggest peduncle, it is the source of most of the mossy fibres.
The middle cerebellar peduncle is very visible (in purple) when you do a cross section of the pons:
Inferior Cerebellar Peduncle
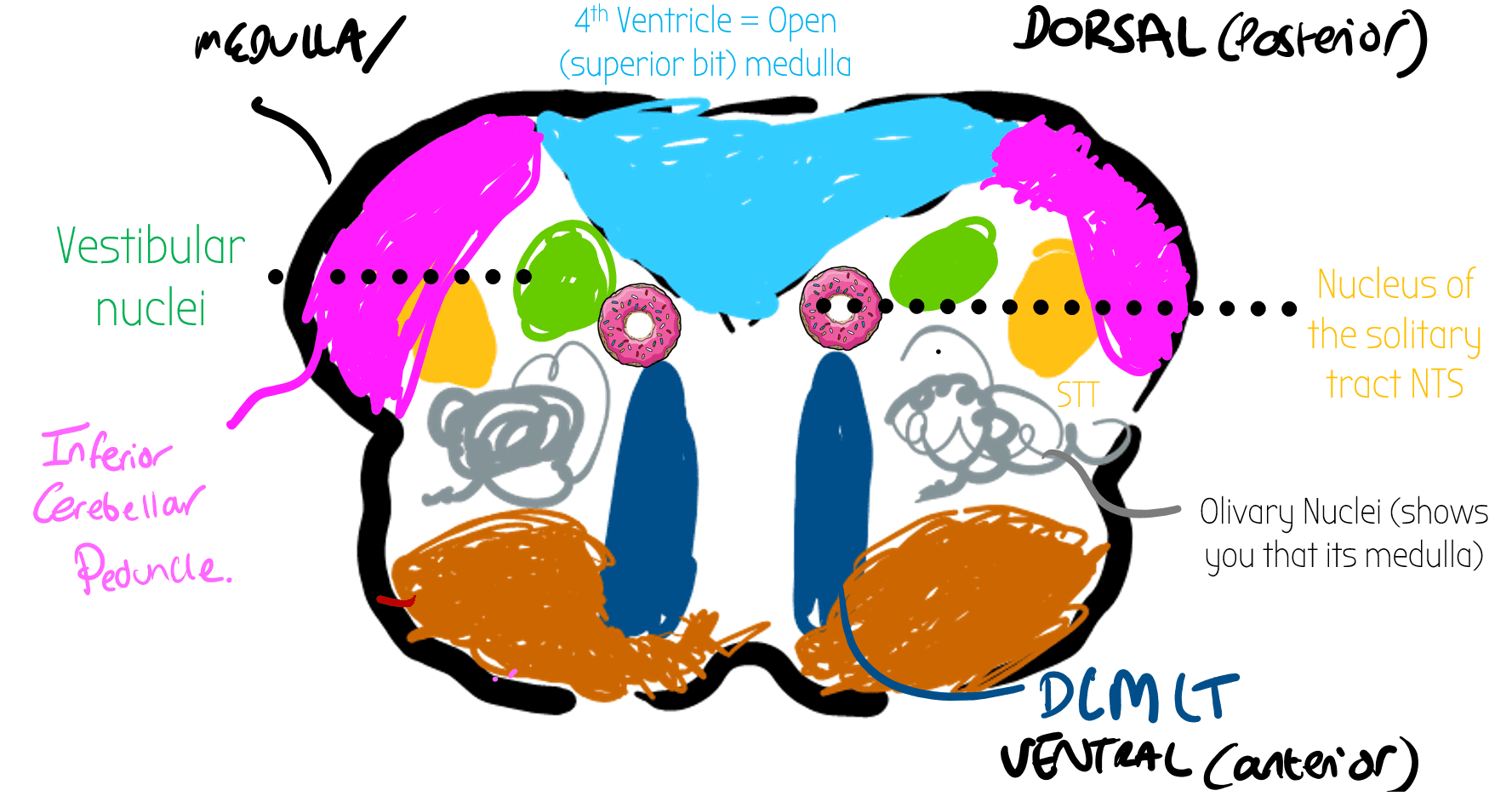
Lowest cerebellar peduncle at the level of the lower pons/very top bit of the open medulla.
The cerebellar peduncles are masses of tissue that connect the brainstem (pons) to the cerebellum
SOURCE OF MOSSY FIBRES FROM DORSOSPINAL CEREBELLAR TRACT
Dorsospinal cerebellar tracts contain proprioceptive information
They travel up from C8-L2 all the way to the inferior cerebellar peduncle, which connects them to the spinocerebellum (intermediate zone around vermis).
From here they turn into mossy fibres and then go to purkinje cells (apart from the dorsospinal cerebellar tracts, most mossy fibres comes from the middle cerebellar peduncle)
Cerebellar Cortex:
Granule Layer
The outer bit of the cerebellum is folded into folia which contain the grey matter. This is the cortex which is divided into three sections. The granule layer is the bottom most section of the cerebellar cortex.
Contains granule cells.
Mossy fibres project onto here.
The granule cells then go upwards to the molecular layer where they split into parallel fibres
INPUTS:
Mossy fibres from pons/dorsospinal cerebellar tract
OUTPUTS:
Mossy fibres synapse onto granule cells which then project upwards into the molecular layer and become thousands of parallel fibres.
LOADS of parallel fibres then go into one purkinje output cell
Purkinje Layer
The purkinje layer is the middle section of the cerebellar cortex.
Contains purkinje cells. These are the main output cells of the cerebellum.
INPUTS:
- Direct input from climbing fibres (arise from the inferior olivary nuclei). 1 climbing fibre : 1 cell
- Mossy fibres split into thousands of parallel fibres. LOADS of parallel fibres connect to ONE purkinje cell
OUTPUTS:
Purkinje cells have efferent fibres to the deep cerebellar nuclei (DCN)
Molecular Layer
The molecular layer is the top/outermost section of the cerebellar cortex.
Contains parallel fibres
At the molecular layer, mossy fibres split into thousands of parallel fibres and then loads of these parallel fibres connect to just one purkinje cell.
The purkinje cell then goes onto the DCN.
Deep Cerebellar Nuclei:
Don't Eat Greasy Food
Dentate | emboliform | Globose | Fastigial
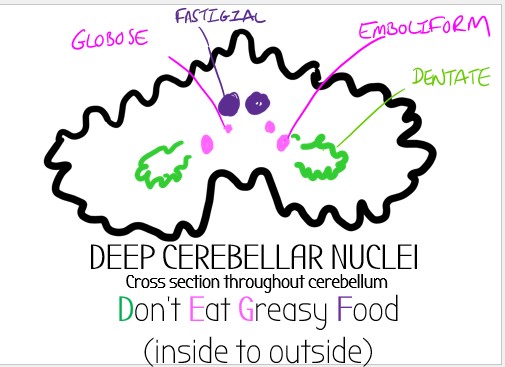
Dentate Nucleus
Outer most nuclei of the DCN (in green)
Main output nuclei of lateral cerebellum (pontocerebellum)
–> Ipsilateral control of movement (via thalamus)
Input from ventral lateral/ventral anterior nucleus of thalamus
Fastigial Nuclei
gfgf
Control balance
Receives info from floccular-nodular lobe and sends axons to
- vestibular nuclei (dorsolateral medulla) via vestibulospinal tract &
- reticular formation
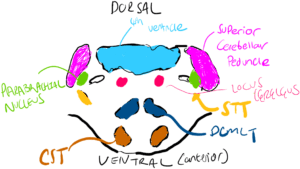
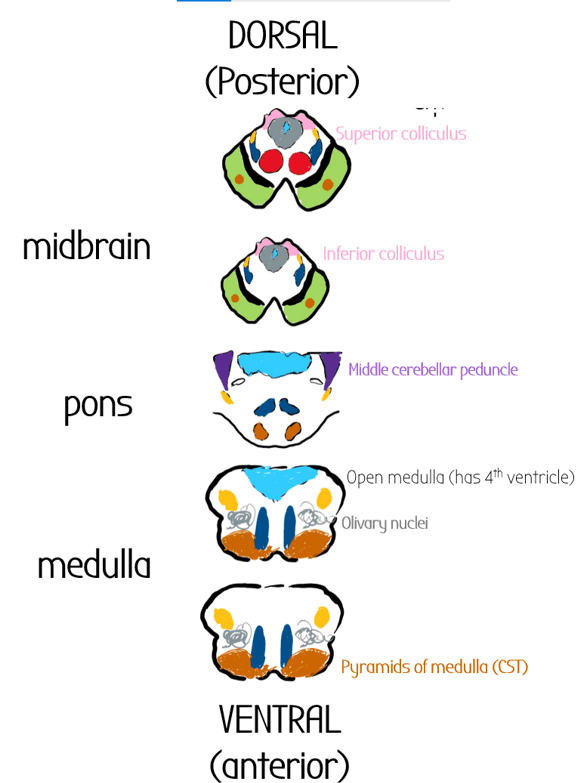
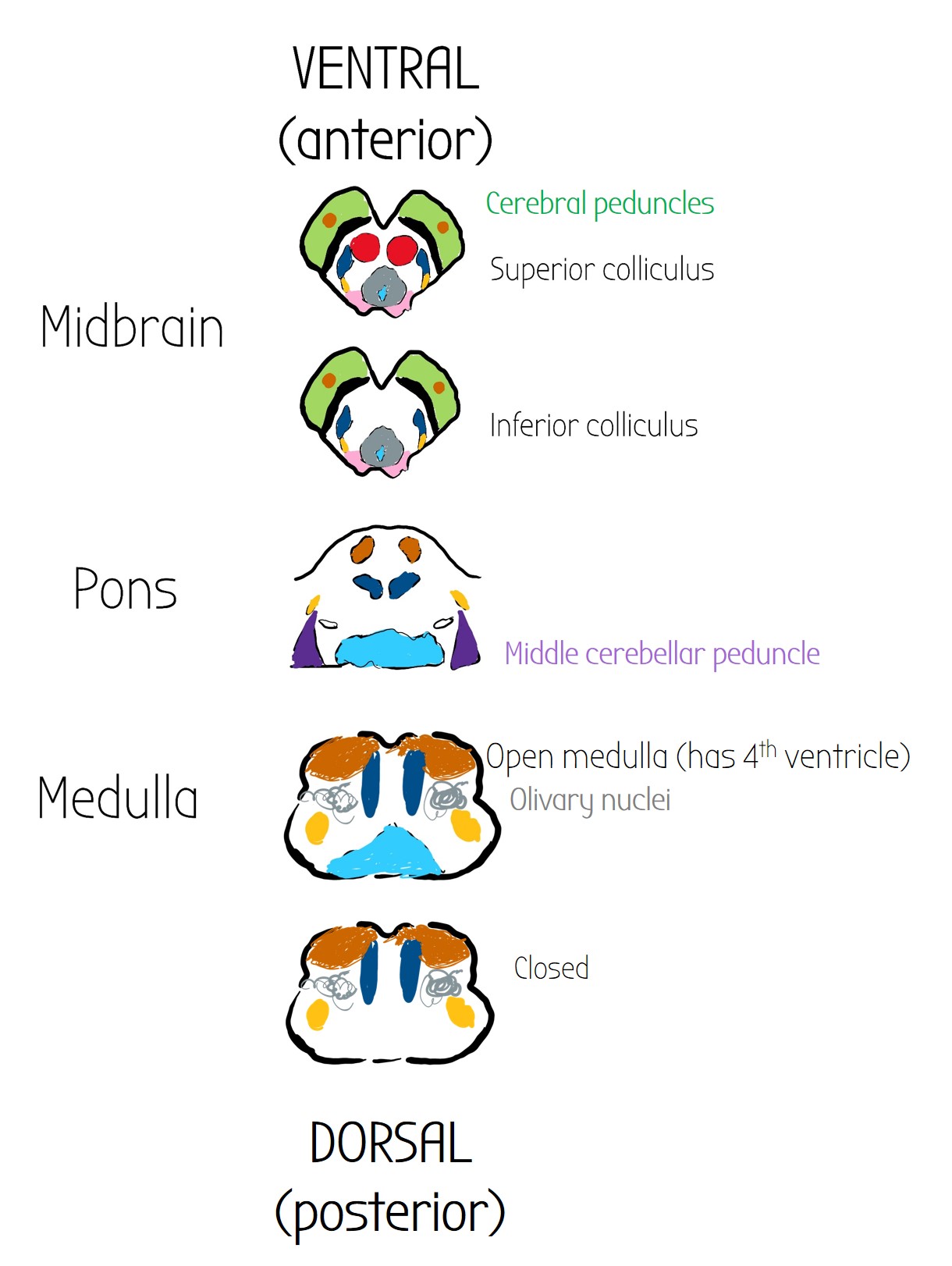
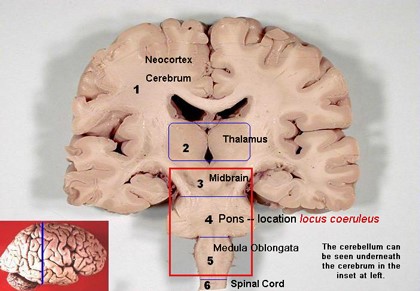
Brainstem
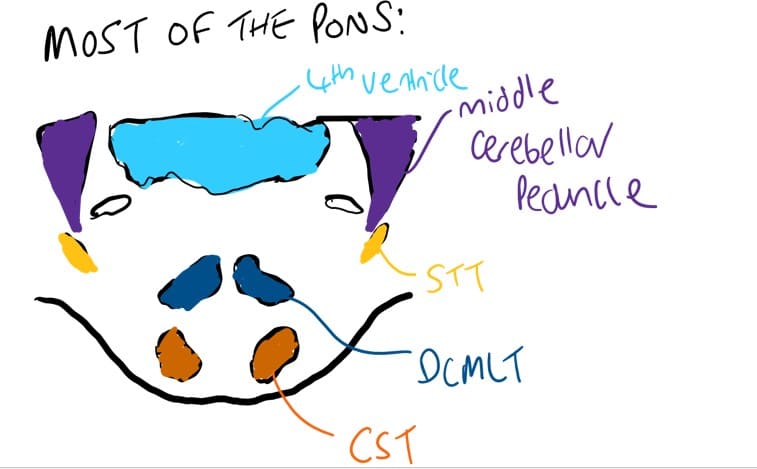
The brainstem is the bit of the brain that connects to the spinal cord – it is responsible for a lot of the non-conscious stuff that keeps us alive.
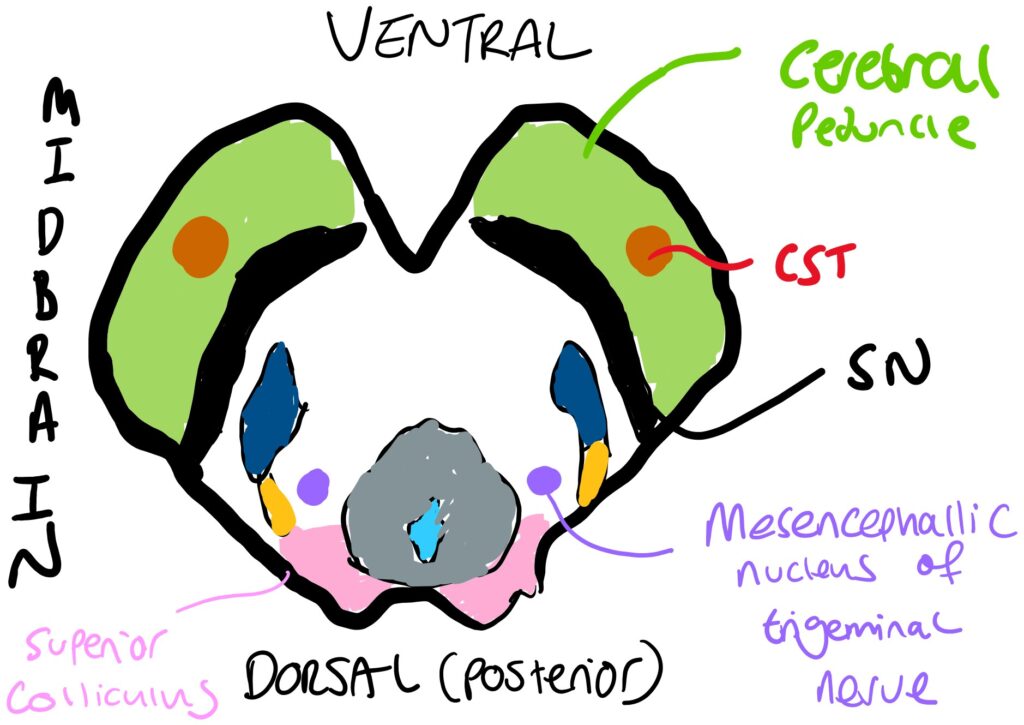
It is made of three sections:
- Midbrain (aka mesencephalon): cerebral peduncles containing CST (shown in green), substantia nigra, red nucleus, DCMLT, STT, midbrain reticular formation, periaqueductal grey, superior/inferior colliculi
- Pons can be divided into layers based on the connections to the cerebellum (mini motor brain) called the cerebellar peduncles
- Superior cerebellar peduncles
- Middle cerebellar peduncles (these are the biggest)
- Inferior cerebellar peduncles – most inferior bit of the pons
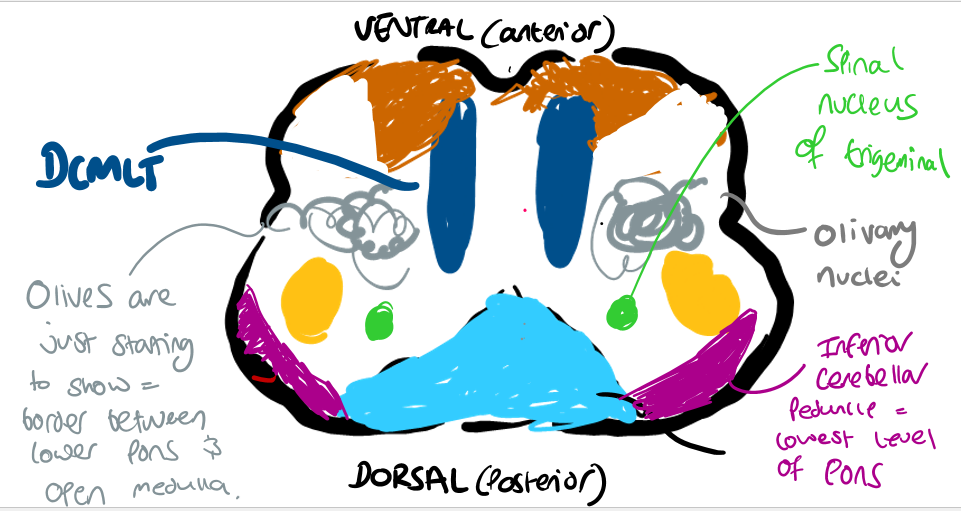
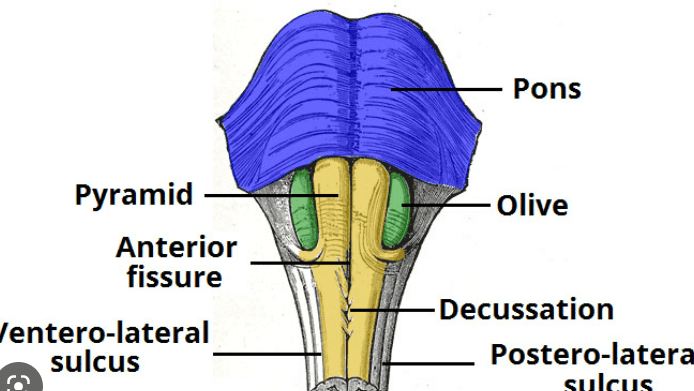
- Medulla the most inferior (caudal – closer to the spinal caud!) bit of the brainstem. Has distinct curly bits which are the olivary nuclei
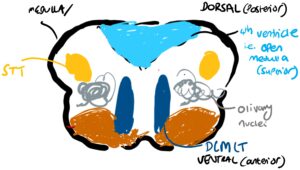
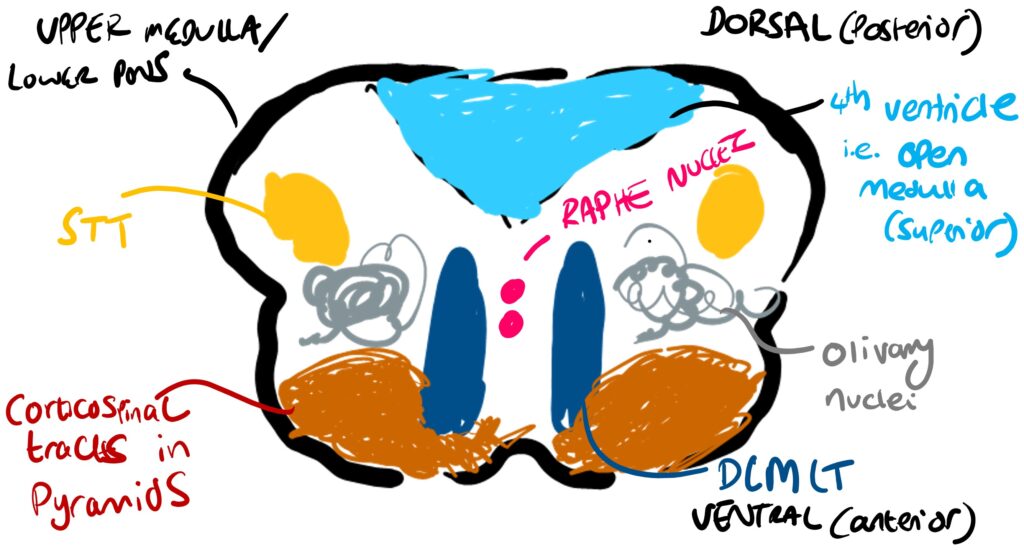
- SUPERIOR: OPEN MEDULLA
The upper bit of the medulla has the 4th ventricle (last collection of CSF in the brain) and is called the open medulla.
- INFERIOR: CLOSED MEDULLA
The 4th ventricle narrows in the lower bit of the medulla to become the central canal of the spinal cord. Therefore there is no more 4th ventricle/fluid stuff in the inferior bit of the medulla
- SUPERIOR: OPEN MEDULLA
After the medulla is the spinal cord
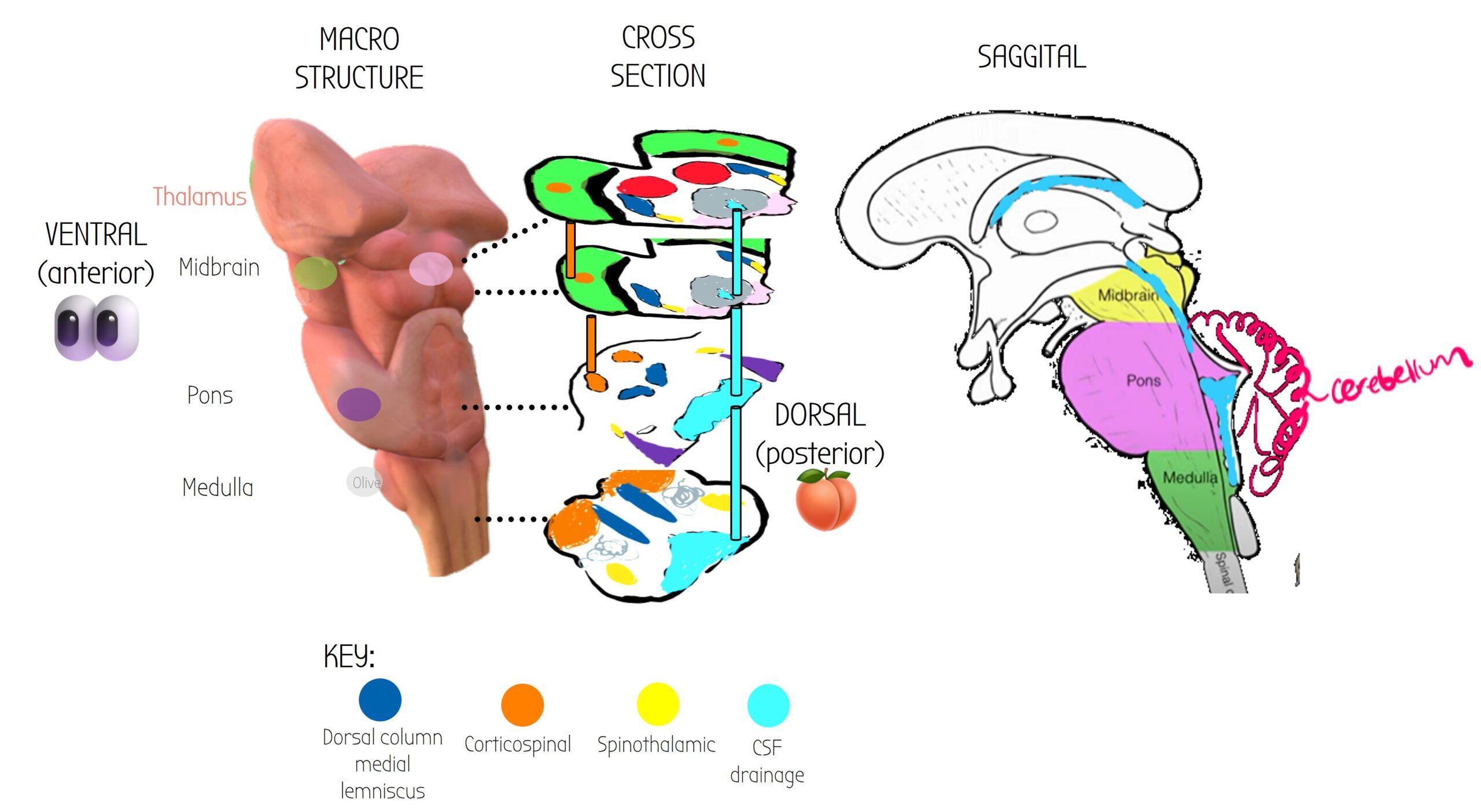
Cerebral peduncles: anterior bits that connect the brainstem to the cereBRUM (the thinking bit of the brain.)
These contain the corticospinal tracts (shown in orange) which control fine movement.
Correlate to the green circle on the macrostuructre - they are found anterior/laterally.
Divided into two levels.
CNIII (oculomotor), IV (trochlear)
Spinothalamic tracts:
Carry nociceptive (pain) & temperature information (ascending tracts).
Crosses at the level of the spinal root - i.e. contralateral information.
Superior Cerebral Peduncles on the midbrain.
This green bit correlates with the bright green on the first two cross sections . These are bits of tissue that connect the brainstem to the main thinking part of the brain (Cerebrum).
Substantia Nigra
Darker neurones found in the midbrain that produce dopamine (DA).
This gets damaged in parkinsons 🙁
The midbrain has 4 bumps on the dorsal side that are visible. Each bump is called a colliculus. There are two at the top, and two at the bottom = superior/inferior colliculi. These make up the tectum which you can see in the saggital view.
- Top two bumpy bois = primary gaze processing 👀
- Bottom two bumpy bois = auditory processing 👂
Correspond with the pink bumps in the first two cross-sectional slices.
Midbrain cross-section at the level of the superior colliculi.
The midbrain has 4 bumpy bits visible at the posterior side- two at the top & two at the bottom called colliculi (superior & inferior).
They are good landmarks. Correlates to the pink circle bit on the midbrain.
Midbrain cross-section at the level of the inferior colliculi.
No red nucleus.
RED NUCLEUS:
The midbrain is divided into two nice levels based on the bumpy bois - superior and inferior colliculi.
The two levels are pretty much identical, except the superior layer contains the RED NUCLEI - which are involved in motor control (extrapyramidal motor control)
This arch at the end of the midbrain is the tectum - the bit of the midbrain that is made of 4 bumpy bois called the superior/inferior colliculi.
DORSAL COLUMN MEDIAL LEMINISCUS
-vibration & proprioception sensory info tracts.
-Crosses at medulla - ie is contralateral.
Periaqueductal grey - the grey matter that surrounds the cerebral aqueduct .
They are able to reduce pain (have an analgesic effect).
Choroid plexus of 3rd ventricle
Produces CSF, which drains out via the cerebral aqueduct into the 4th ventricle.
Cerebral aqueduct
CSF flows from choroid plexus of 3rd ventricle into the cerebral aqueduct which passes through midbrain and ends in the 4th ventricle at the level of the pons.
4th Ventricle
The 4th and final place where fluid (CSF) collects in the brain. This is found at the same level of the pons.
Middle Cerebellar Peduncle
Correlates with purple bit at pons cross section
The pons connects with the cerebellum (the motor mini-brain) via bits 3 of tissue called peduncles. They are located laterally, the largest cerebellar peduncle is the middle cerebellar peduncle.
Middle Cerebellar Peduncle
Correlates with purple blob at pons macro-section
Connects pons to the cerebellum (motor mini-brain).
Contain mossy fibres
4th Ventricle
Cerebral aqueduct now becomes a big juicy space filled with yummy CSF AKA 4th Ventricle. This is found at the same level of the pons.
4th ventricle also has a choroid plexus that allows for production of/drainage of CSF.
Corticospinal tracts
Descending tracts that carry info for fine motor control continue at the ventral (anterior) side.
Corticospinal tracts decussate at the pyramids.
Cerebral aqueduct
Pyramids
At the medulla, the corticospinal tracts (descending controls for fine motor) become big chunky things at the anterior (ventral) side, called pyramids.
The pyramids CROSS OVER, meaning that from now on, the corticospinal tracts control the contralateral side of the body.
4th Ventricle
Olive
At the medulla there are lateral bulges of tissues called olives which contain the olivary nuclei (contain climbing fibres)
Superior cerebellar peduncle
Contains efferent output fibres from the mini-motor brain (cerebellum)
Olivary nuclei
contain climbing fibres
Medial Lemniscus
At medulla, the medial lemniscus (carries vibration & proprioception info) is quite anterior and close to the midline. As it goes up into midbrain it becomes more dorsal.
The cross sections in the diagram above have been orientated as if you are standing behind someones brainstem and looking at them (posterior view).
Normally neuroanatomy diagrams shows cross-sections the other way but that is harder to visualise – so dont be confused!
Nuclei
Location
Function
Connections & Neurotransmitters
Pathologies
Midbrain nuclei
- Red nucleus
- Superior colliculi
- Oculomotor
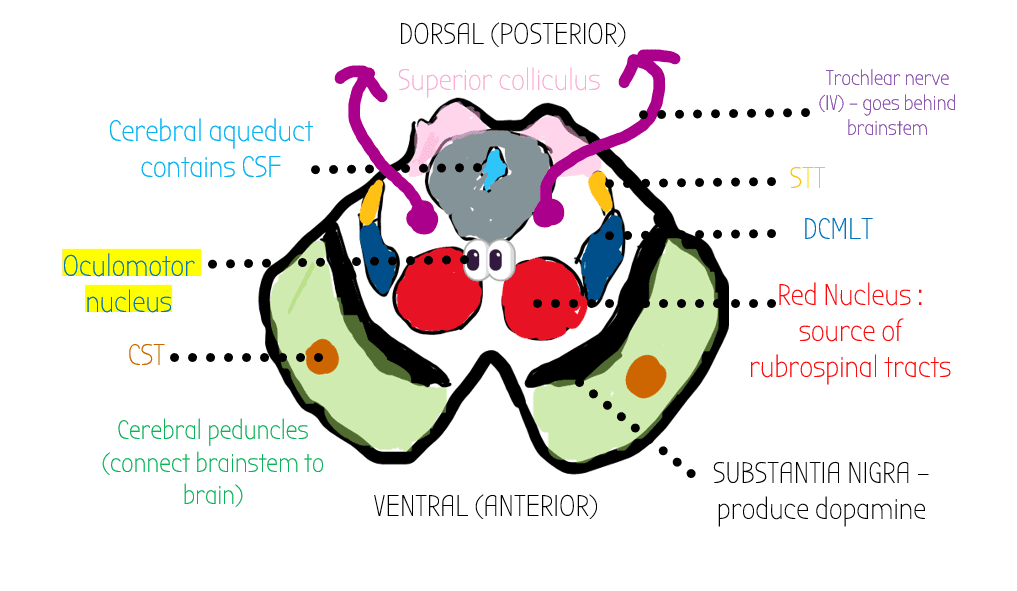
The oculomotor CNIII nucleus contains a parasympathetic bit called the Edinger-Westphal nucleus
Pupillary Light Reflex (high yield)
–> Shine a light into one of someone’s eyes, BOTH their pupils will constrict:
- Ganglion cells in the retina detect light
- Info carried by optic nerve
- Pretectal nucleus goes to both edinger-westphal nuclei
- Info goes to Edingher-westphal nucleus on contralateral side
- Short Ciliary nerves = sympathetic ganglion –> oculomotor
- Sphincter pupillae muscle causes pupil to constrict. This is innervated by CNIII
If you have a CNIII third nerve palsy (down and out), the sphincter pupillae muscle won’t be able to contract, so therefore the pupil will be fixed and dilated 🙁
Locus cereleus
Just in front of superior cerebellar peduncle, near the 4th ventricle
Have an analgesic effect on:
- pain 🤕
- wakefulness 😴
- memory 🧠
NA (noradrenergic connections) all over the brain
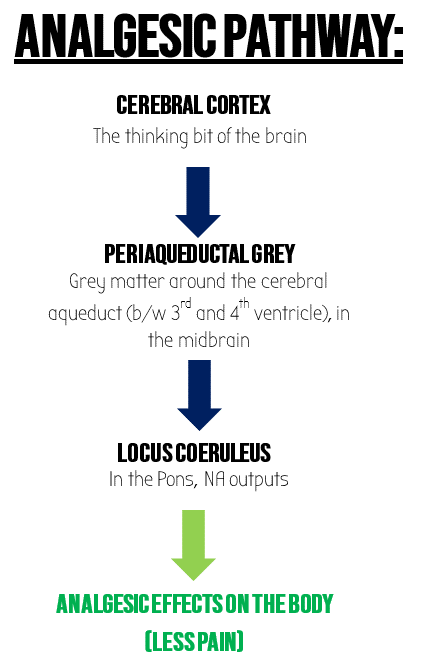
Locus coereleus releases NA which acts on a2-adrenoreceptor.
This is part of inhibitory pain controls 🙂
Inhibitory pain controls of locus coereleus lost in chronic pains
In contrast to the locus coereleus, the rostral ventral medial medulla (RVM medulla) WORSENS PAIN BY RELEASING 5HT 🙁
Trigeminal sensory nuclei
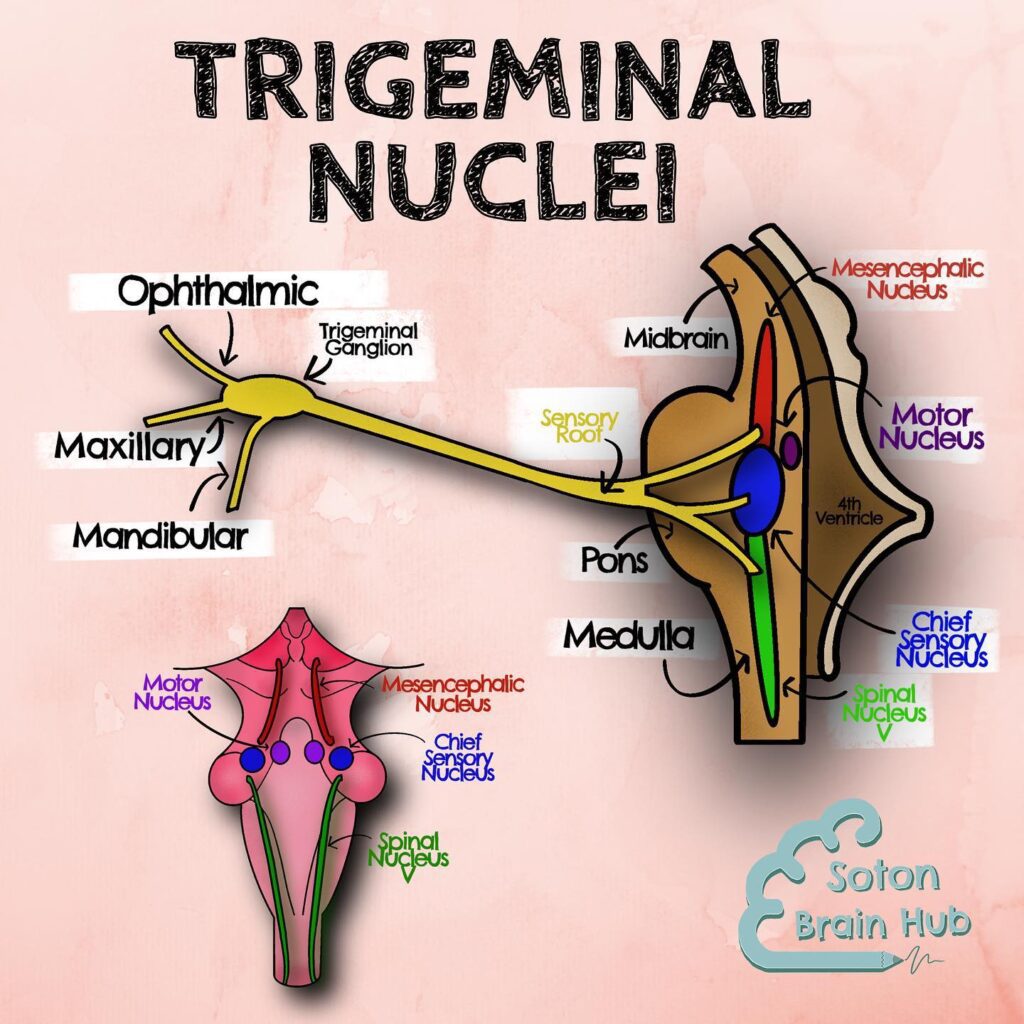
The three sensory branches of the trigeminal nerve (V) comes into the brainstem via the trigeminal ganglion.
- The ganglion then splits up into three separate nuclei
– mesencephalic nucleus in rostral end (top bit – rostral is near the NOSTRIL) in midbrain,
-Chief nucleus in middle (upper pons)
= discriminative touch of face
-Spinal nucleus at the caudal end of the brainstem (continous with the dorsal horn of spinal cord – hence called SPINAL!). The spinal nucleus is (dorsal, lateral) at the level of the lower pons/ upper open medulla
Chief nucleus of trigeminal nerve = discriminative touch info about the face via AB fibres
Spinal nucleus controls nociceptive (pain sensing) bits of trigeminal nerve via C fibres
Anterior 2/3 of tongue supplies somatosensory information via lingual nerve (mandibular branch) to spinal nucleus
- 🦠 Shingles ==> post herpetic neuralgia (i.e. nerve pain after you get herpes) -often spreads unilaterally on one side of the route of a section of trigeminal nerve
- 🩸 The superior cerebellar artery can irritate the trigeminal nerve and cause trigeminal neuralgia – extreme pain in face
SPINAL NUCLEUS STROKES
- 🩸 Spinal nucleus supplied by AICA/PICA
- ⚠️ AICA/ PICA STROKE/LESIONS WILL DAMAGE SPINAL NUCLEUS ==> CAUSE LOSS TO TRIGEMINAL FUNCTIONS
- ⚠️ Ipsilateral face anaesthesia (numbness when chewing)
Nuclei
Location
Function
Connections & Neurotransmitters
Pathologies
Medial Leminiscus
Found throughout brainstem.
Open medulla:
Receives sensory info about vibration, proprioception & discriminative touch from contralateral side of the body
( fibres ipsilateral at spine but cross at medulla aka hindbrain)

These fibres go to ventral posterior nucleus of thalamus (which is quite close to the brainstem). From here info gets relayed to somatosensory areas of cerebral cortex (e.g. post-central sulcus) via RECICIPIRICAL CONNECTIONS
The post central sulcus in the cerebrum helps work out what objects are via discriminative touch : STEROGNOSIS
• TABES DORSALIS – most common form of neurosyphilis – stamping gait due to lack of proprioception in dorsal column
• FRIEDREICH’S ATAXIA: genetic degenerative of DC tracts & spinocerebllar
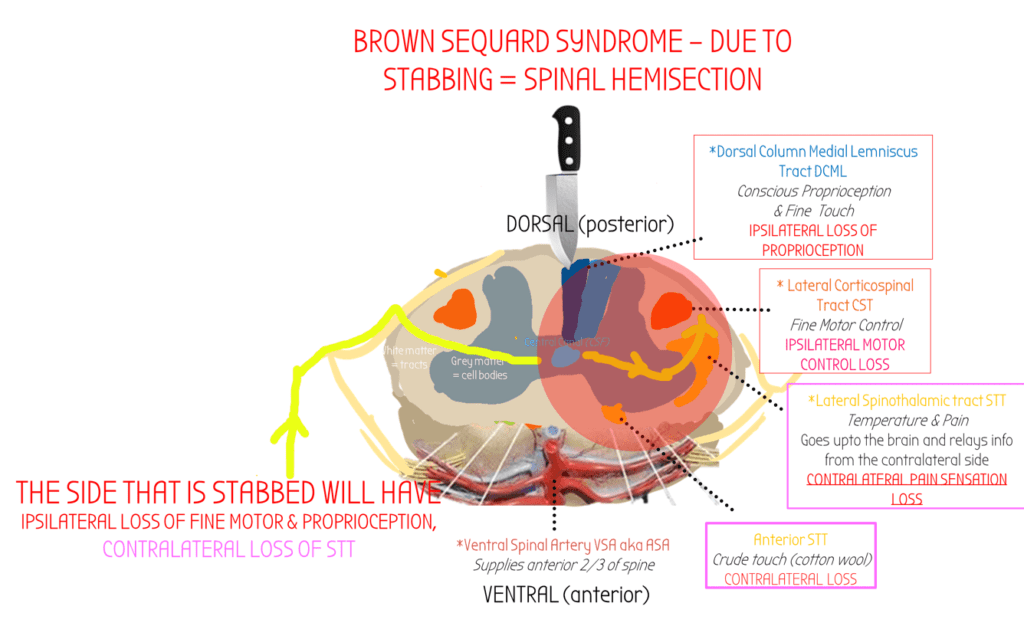
• BROWN-SEQUARD SYNDROME – hemisection of spinal cord often due to stabbing – loss of ipsilateral touch and proprioception sensation on side of inury due to cutting of DCML
Complete loss of both nociceptive (spinothalamic) & proprioceptive (DCML) sensation at the level of the injury.
Raphe Nuclei Part of reticular activating system
There are several nuclei that make up the Raphe nuclei that are found throughout the brainstem.
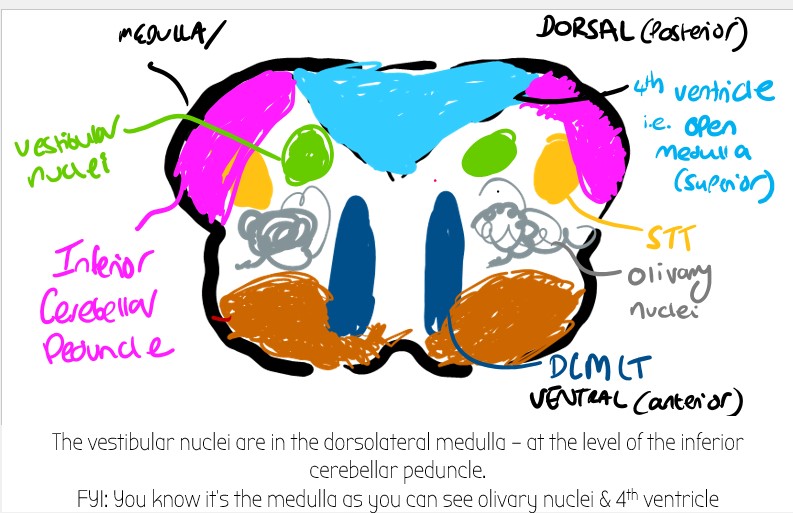
Raphe Magnus is found somewhere at the lower pons/upper bit of the medulla (open medulla) – i.e. where there is the 4th ventricle, and olivary nuclei.
Modulate pain
Also modulates the mesencephalic locomotor region (MLR) – which controls walking speed. 🚶♂️–>🏃♂️
Use 5HT (serotonin) as a neurotransmitter.
Medial Longitudinal Fasiculus
Open Medulla
Integrates all the eye nerves together (CNIII, CNIV, CNVI) & connects them to CNVIII (8) – for vestibulo-ocular reflex.
Receive info DIRECTLY from the fastigial nucleus (DCN) from the floccular-nodular lobe in cerebellum – originally from CNVIII (8)
PICA Stroke – balance problems/nystagmus
Vestibular nuclei
Dorsolateral medulla.
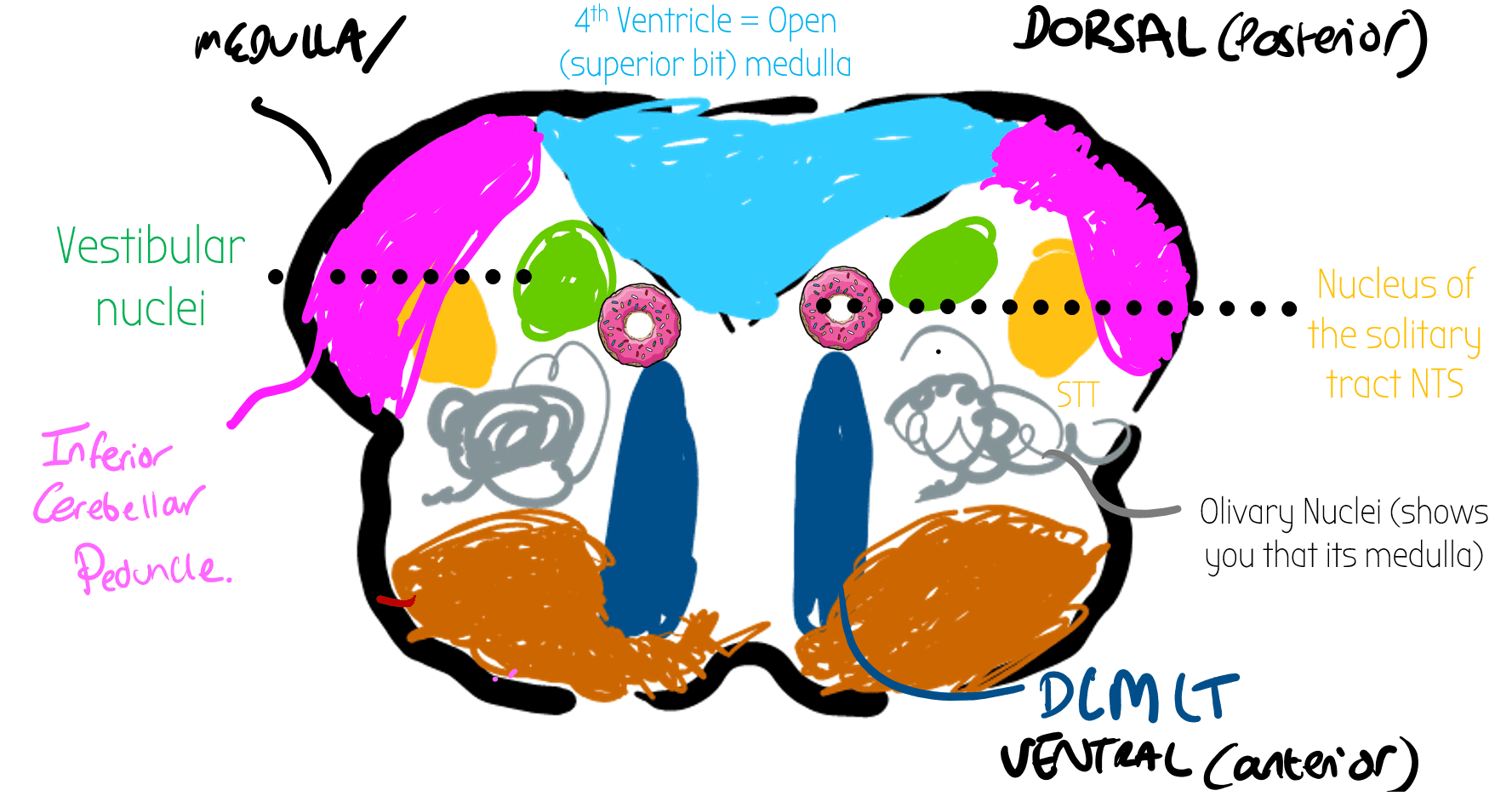
Receive information about balance
Receive info DIRECTLY from the fastigial nucleus (DCN) from the floccular-nodular lobe in cerebellum – originally from CNVIII (8)
PICA Stroke – balance problems/nystagmus
🍩 Nucleus of the Solitary Tract NTS 🍩
Dorsolateral open medulla (superior bit of the medulla).
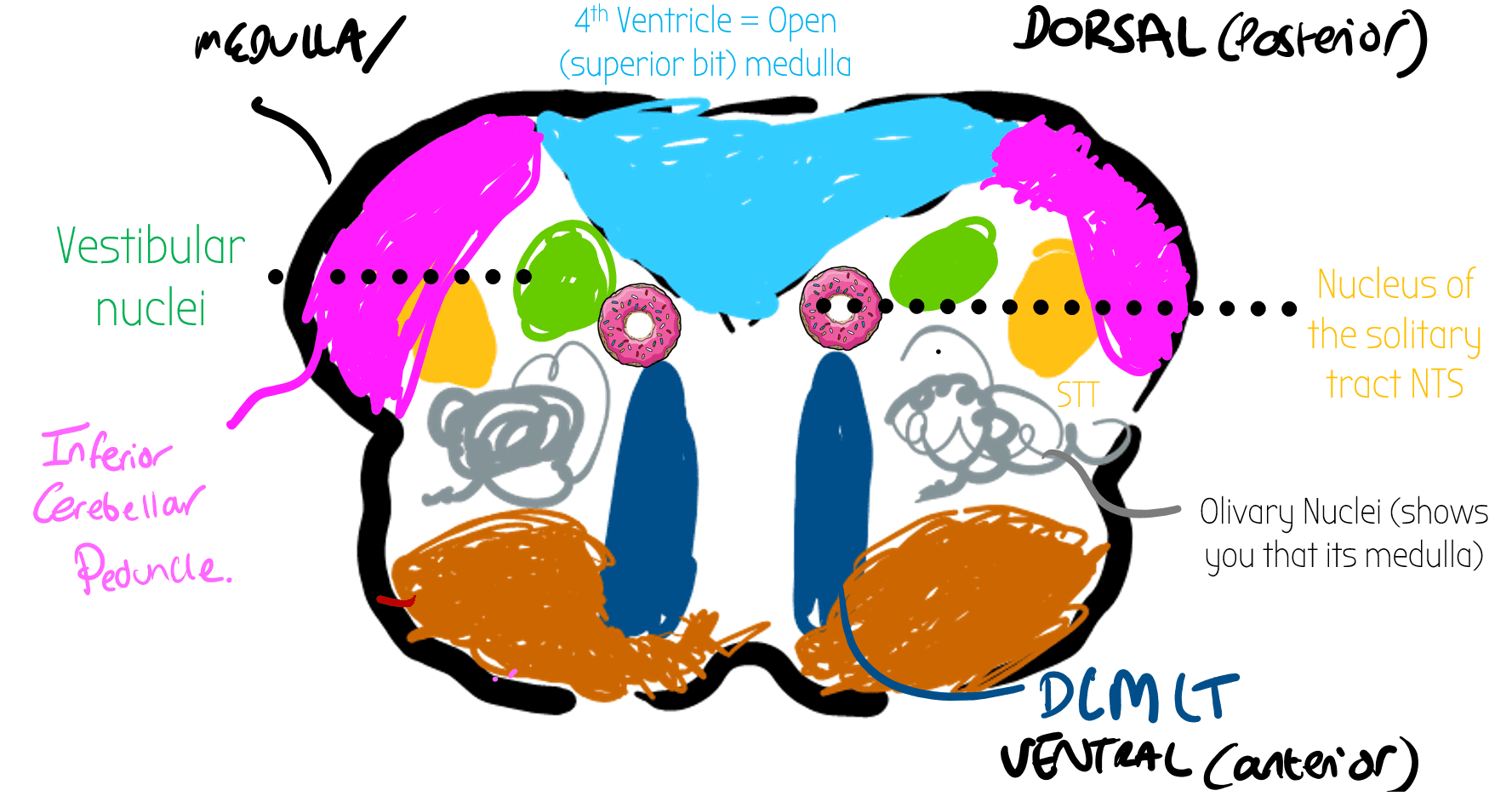
Baroreceptor & taste
Input:
- 🫀 Baroreceptors in aortic arch/ carotid sins
- NTS decreases BP by increasing parasympathetic drive & leading to the rostral ventral lateral medulla RVLM to be inhibited (decreasing sympathetic drive)
Also has endings of visceral afferent fibres of taste & gut – THINK! WHEN
🫒 Olive
Anterior swelling of the medulla
Inferior Olivary Nuclei: Source of all climbing fibres which contain error signals and go to the cerebellum, projecting directly onto the purkinje cells
Superior Olivary Nuclei: auditory processing & integration
Climbing Fibres
- Carry Error Signals to the cerebellum e.g. retinal slip
- SOURCES:
- ALL ARISE FROM THE INFERIOR OLIVE
- Olive trees climb!
- ALL ARISE FROM THE INFERIOR OLIVE
- ROUTE:
- Fibres come from the inferior olivary nuclei in the olives in the medulla
- Cross the midline (CONTRALATERAL) and go to inferior cerebellar peduncle
- From here, they form climbing fibres
- These climb directly to the purkinje cell (without splitting into parallel fibres)
- PURKINJE CELL OUTPUT
- ONE CLIMBING FIBRE TO ONE PURKINJE CELL (1:1)
- Purkinje cell has one output fibre to the deep cerebellar nuclei to make adjustments
Fibres, Nerves & Tracts
Auditory processing: cochlear nuclei, MGN, superior & inferior colliculus , superior olivary nuclei.
Auditory Summary Video (9 mins)
Auditory Processing in Depth (50 mins):
Eye Muscle Movements:
Visual Field Pathways Video:
Interactive Version of Visual Processing:
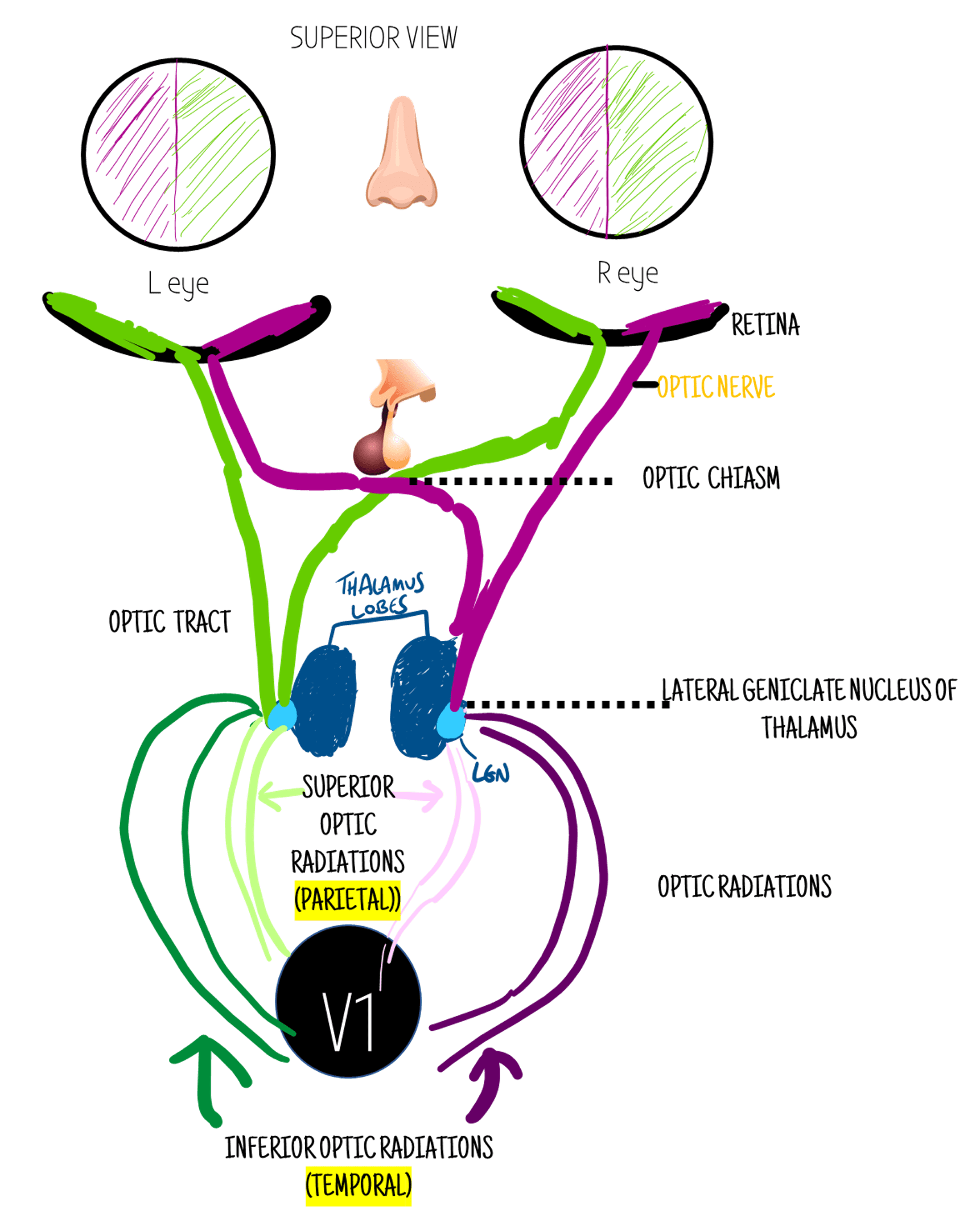
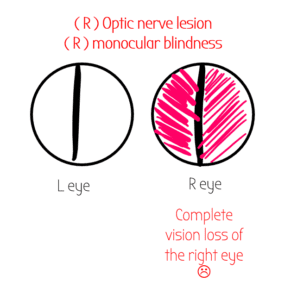
Optic Chiasm Damage
Often due to pituitary adenoma (tumour of pituatary gland) - HIGH YIELD - ESR LINK!
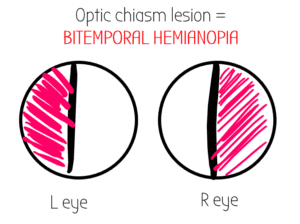
The outer visual fields (temporal fields) cross at the optic chiasm - so damage here causes loss of the lateral/outer/temporal fields
Optic Nerve
Info leaves the retina from both visual fields through a bundle of fibres called the optic nerve. The optic nerve then travels into the brain.
Each eye has its own optic nerve - CNII
Occipital lobe/ V1 Lesion

-PCA Stroke
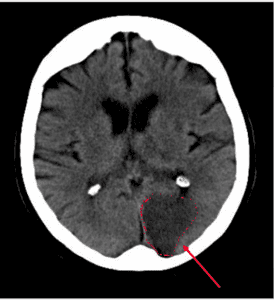
This CT scan shows a stroke on the patient's LEFT side.
PCA stroke may also affect CNIII (oculomotor) - Weber's Syndrome
Optic Tract
The optic nerve turns into the optic tract after the optic chiasm.
The optic tract contains the visual info from the contralateral visual field - ie the left optic tract contains the info for the right visual field (green) - because of the crossing at the retina.
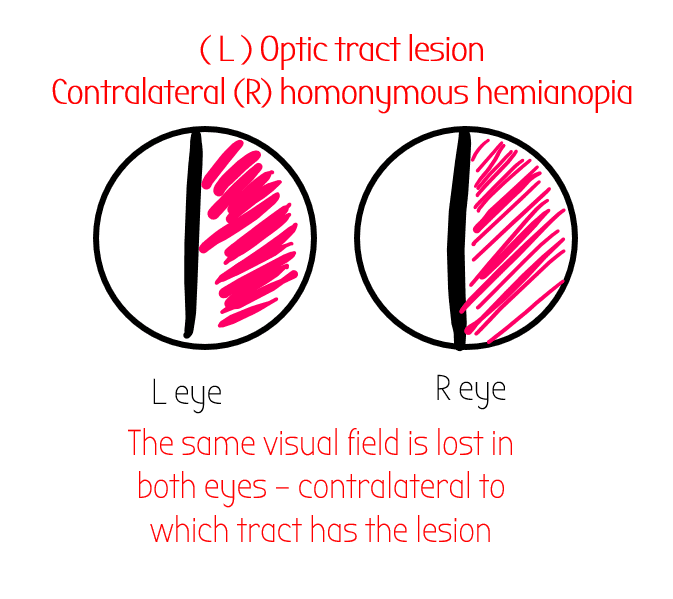
🩸 Optic tract lesions often occur in MCA strokes
Often occurs with Relative Afferent Pupillary
Defect
---> Test for by swinging the shining light. The patient should not normally have RAPD - it’s a bad thing!
Retina
At the retina, the visual field info crosses to the opposite side - e.g. the temporal fields connect to the inner bit of the retina
Lateral Geniculate Nucleus
Both lobes of the thalamus have a lateral geniculate nucleus - this takes in info and then has reciprocal connections (optic radiations) to the visual cortex - V1.
Optic Radiations
After the optic tracts have gone to the thalamus, they split into 4 optic radiations - 2 superior/& 2 inferior branches.
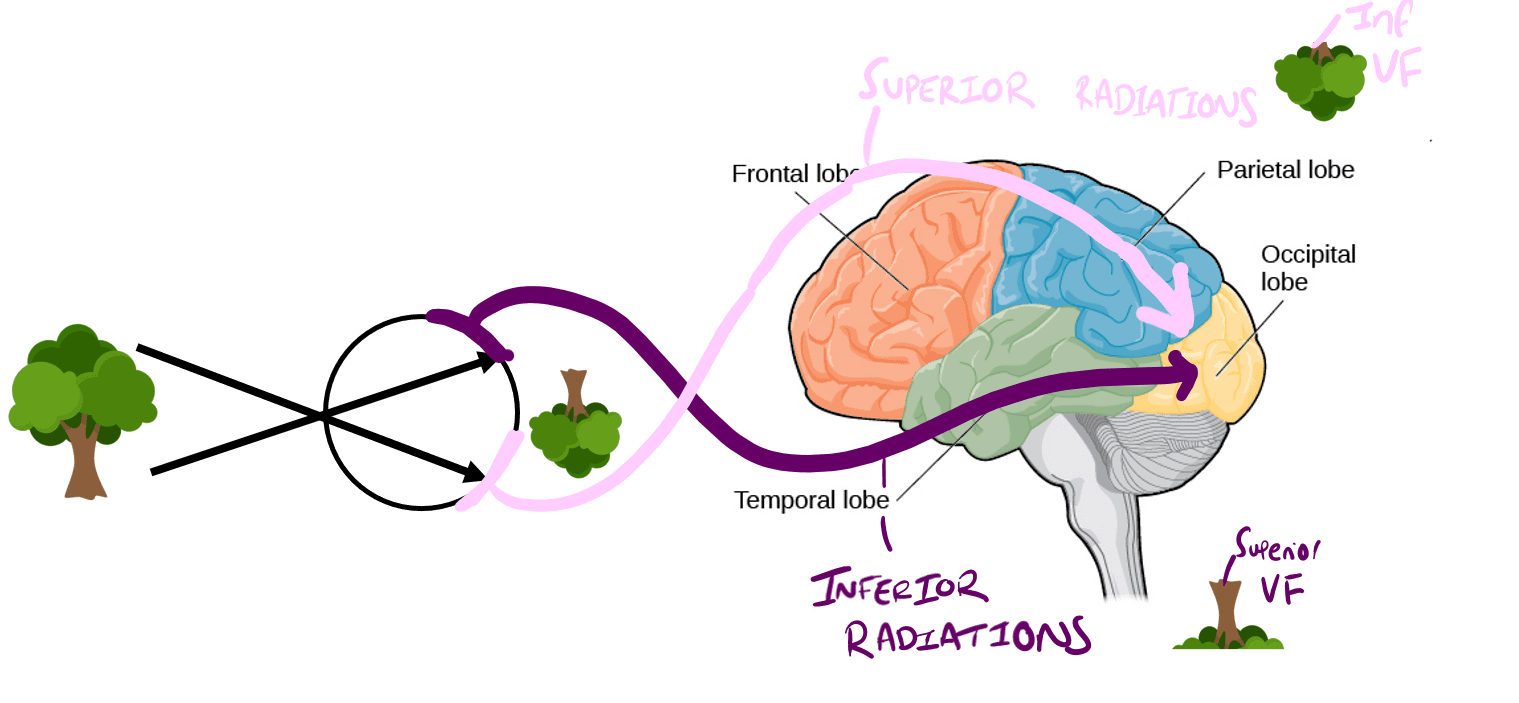
- Superior optic fibres pass over the parietal lobe - carry info about INFERIOR VF
- Inferior optic radiations - pass through temporal lobe - carry info about SUPERIOR VF
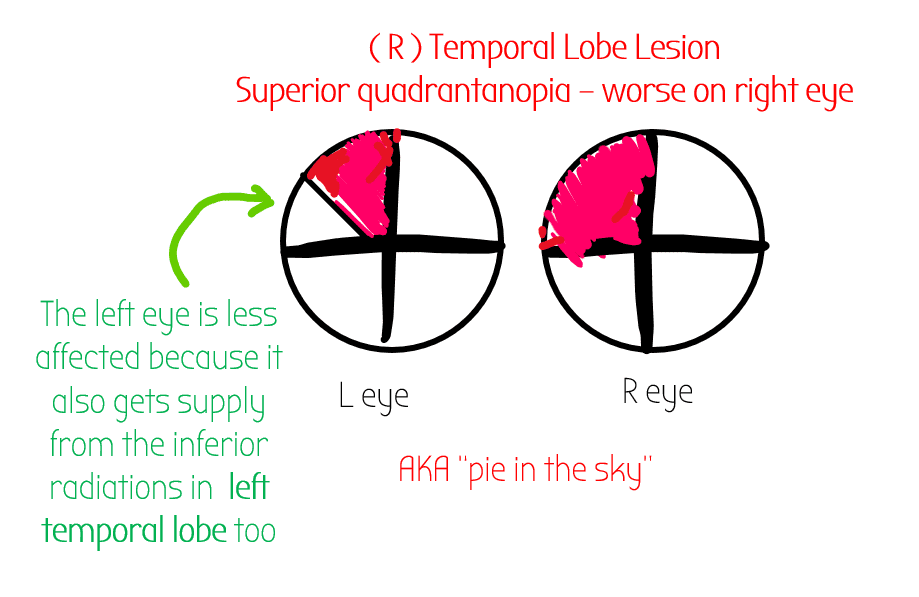
Inferior Optic Radiation
Come from LGN, go through the temporal lobe.
Contain info about the superior visual fields.
When the temporal lobe is damaged, you will get loss of the contralateral visual field BUT it will only be in the superior quadrant
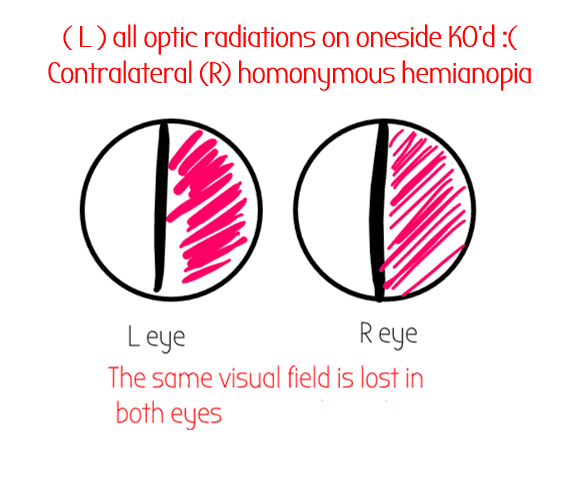
Lesion in both superior and inferior optic radiations:
Tracts
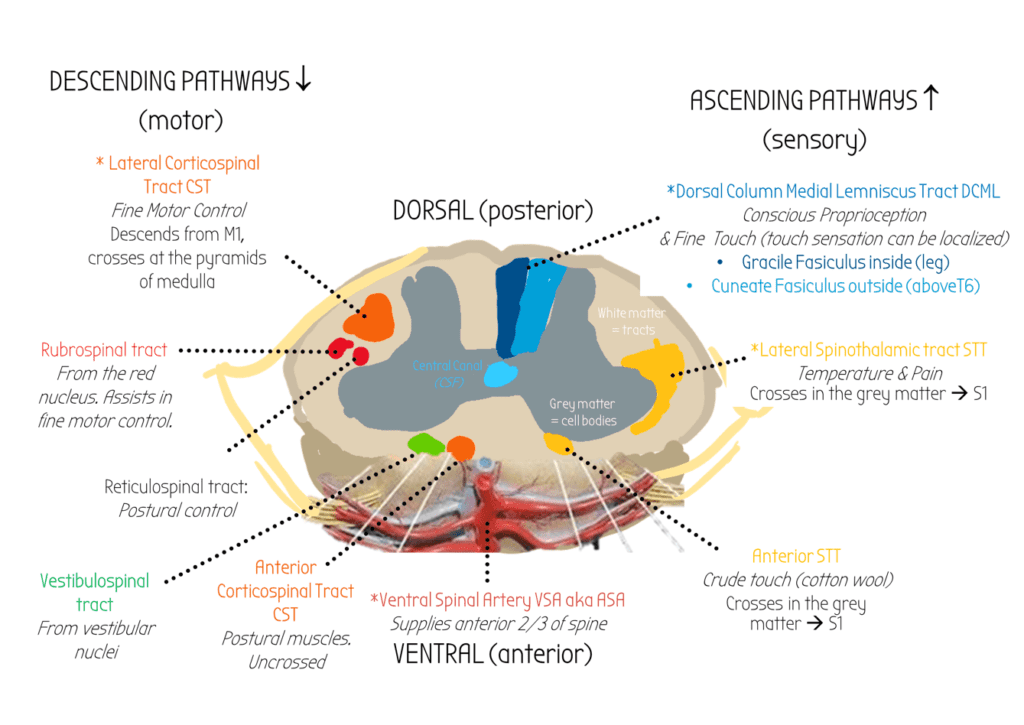
High yield tracts have a *
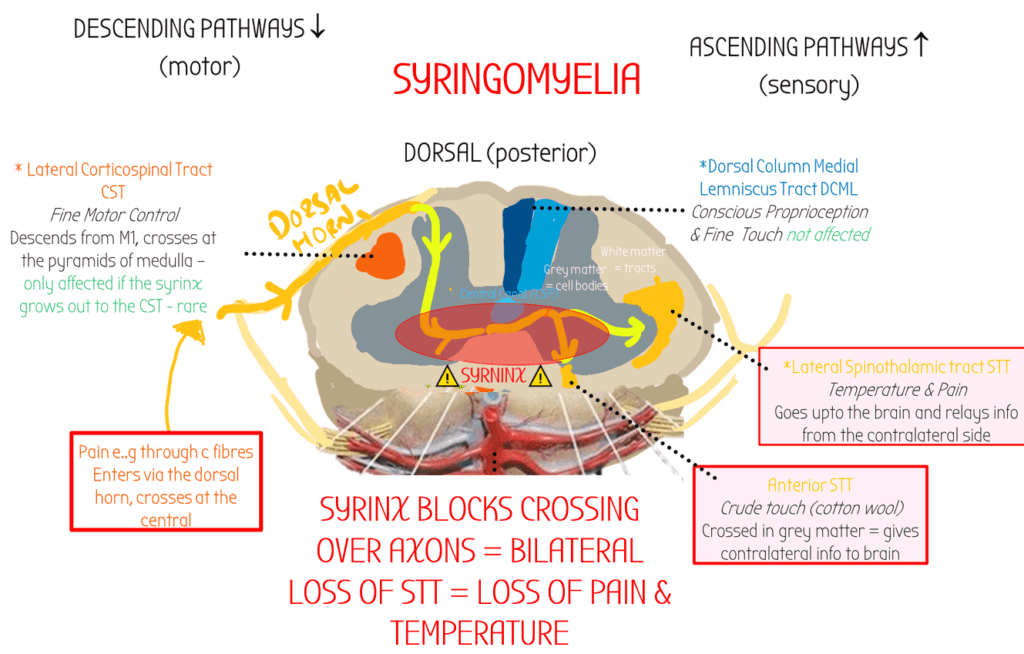
Syringomyelia occurs when a fluid filled cyst goes in the spinal central canal & blocks crossing over axons.
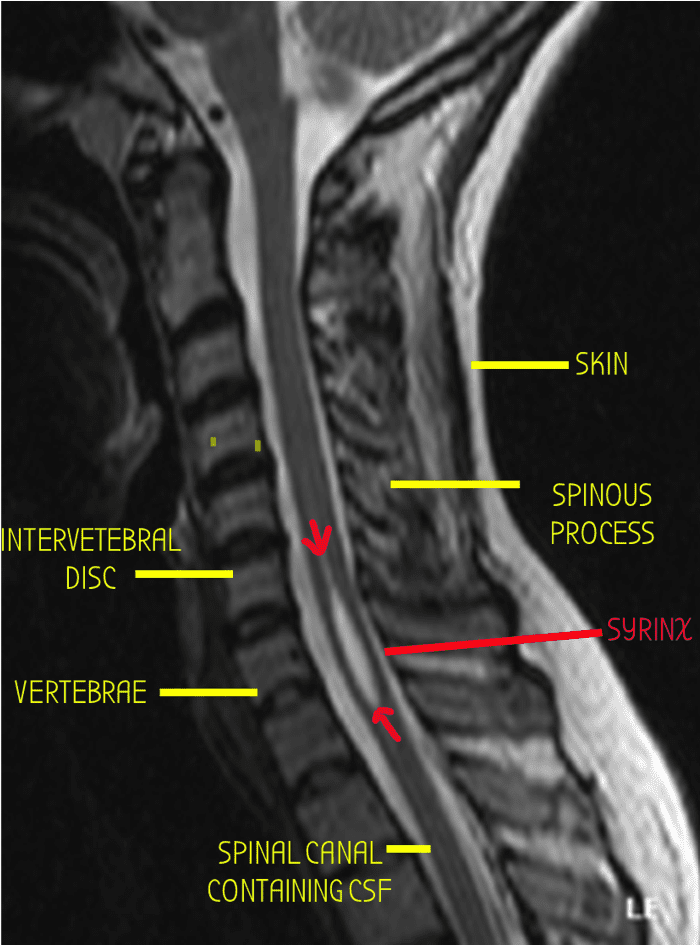
Complete loss of both nociceptive (spinothalamic) & proprioceptive (DCML) sensation at the level of the injury
Tract
Pathway
Function
Crossed over?
Pathologies
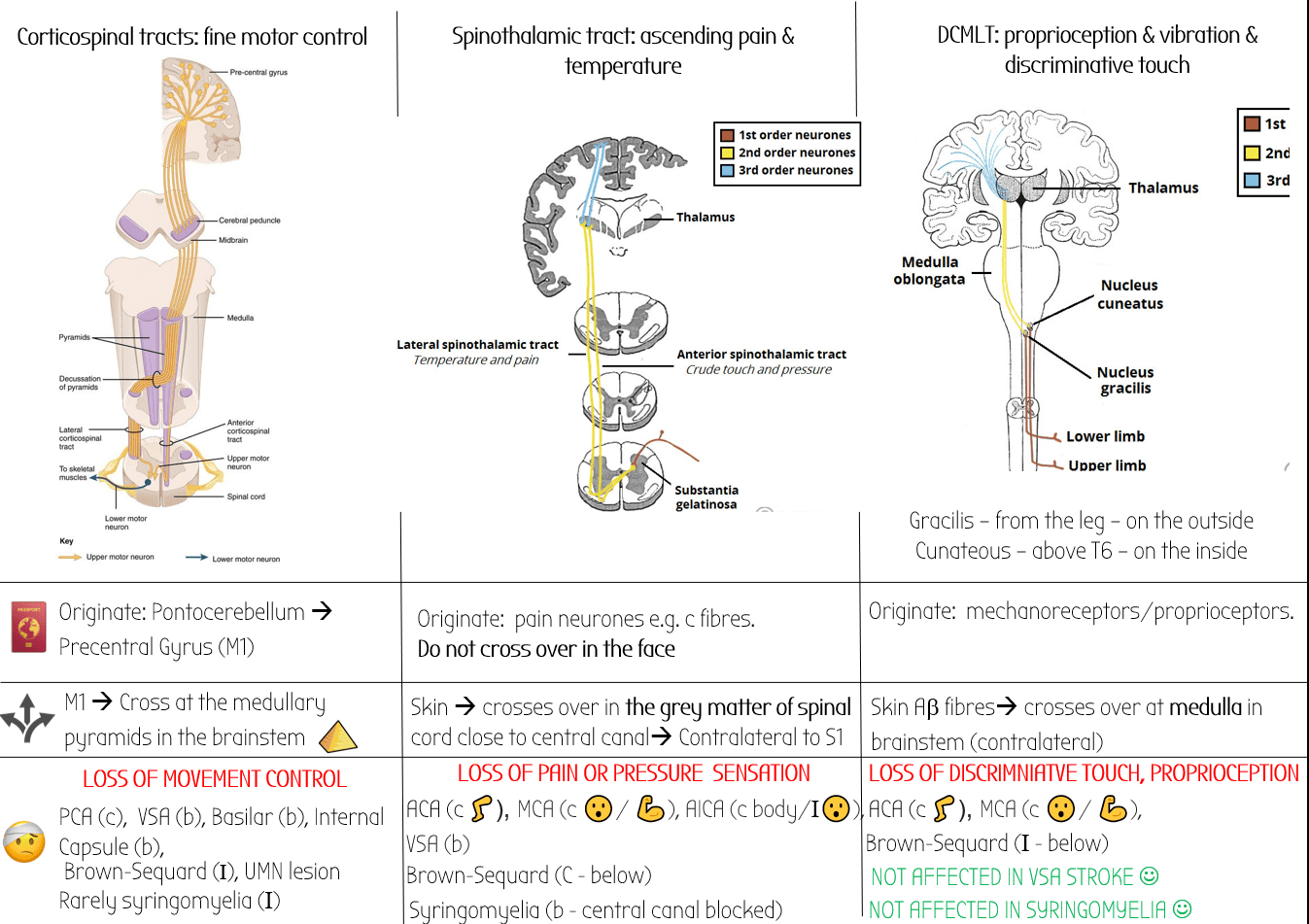
Corticospinal Tract (CST)
Pathway
Motor Tracts
Lateral corticospinal: fine motor control – wiggling fingers
Ventral Corticospinal: postural muscle
Lateral Corticospinal Tracts cross over at the pyramids of the medulla
If (lateral) corticospinal tracts are damaged after they have crossed at the pyramids of the medulla, then symptoms will be IPSILATERAL (i.e. if damaged in the spine) . If damaged before they cross (in the brain/UMN), symptoms are contralateral
Strokes:
-PCA (contralateral hemiplegia – mostly in face)
–Brown-Sequard Syndrome
Hemisection of spinal cord often due to stabbing
at the level of & below the lesion: IPSILATERAL fine motor los
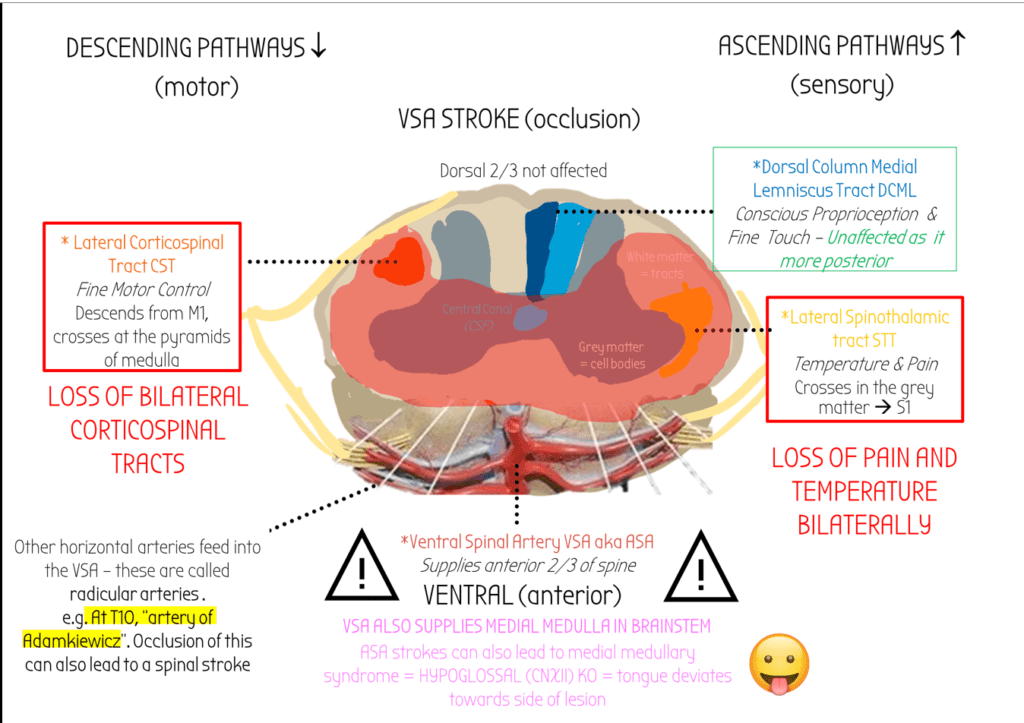
Ventral (anterior) Spinal Artery Stroke
–Syringomyelia rarely affects the CST – if the syrinx grows outwards to the lateral CST.
UMN ALWAYS INVOLVE CORTICOSPINAL TRACTS. LOSS OF CST IN UMN LESIONS CAUSES HYPERREFLEXIA
Spinothalamic Tract (STT)
Pathway
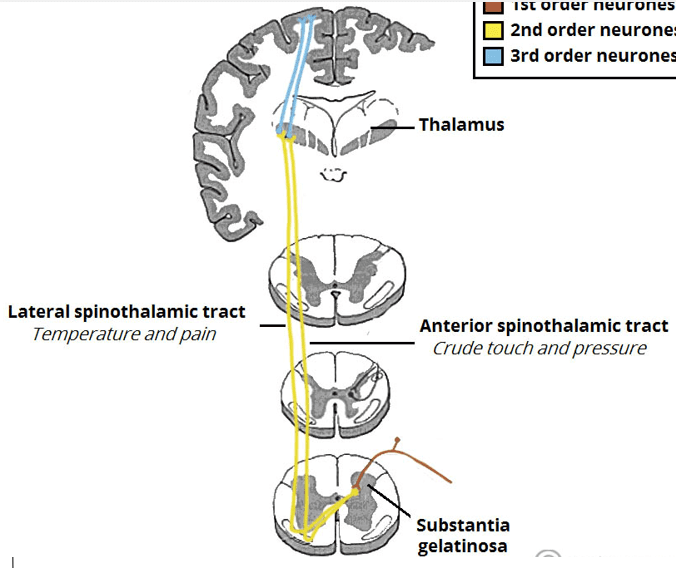
Pain/temperature info enters via the dorsal column, goes through the grey matter and crosses-over near the spinal canal, and then goes upto S1.
Therefore carries contralateral pain/nociception/temperature info
Pain / Temperature Sensory Tracts
Lateral STT: contralateral pain ( nociception) & temperature
Anterior STT: contralateral crude touch – can be tested with a cotton wool.
STT can be removed in a procedure called ventrolateral cordotomy to stop terminally ill pateitns from feeling pain
Both anterior/lateral STT cross at grey matter in spinal cord
LOSS OF PAIN OR PRESSURE SENSATION
Strokes:
ACA (contralateral loss in leg 🦵),
MCA (contralateral loss in face 😮/ arms 💪),
AICA (contrateral loss in body/Ipsilateral loss in face😮),
Bilateral loss in Anterior Spinal Artery stroke
Brown-Sequard – contralateral loss below lesion, bilateral at level of lesion
Syringomyelia – bilateral as both sides are blocked from crossing over by the syrinx
Dorsal Column Medial Lemniscus Tract
Pathway
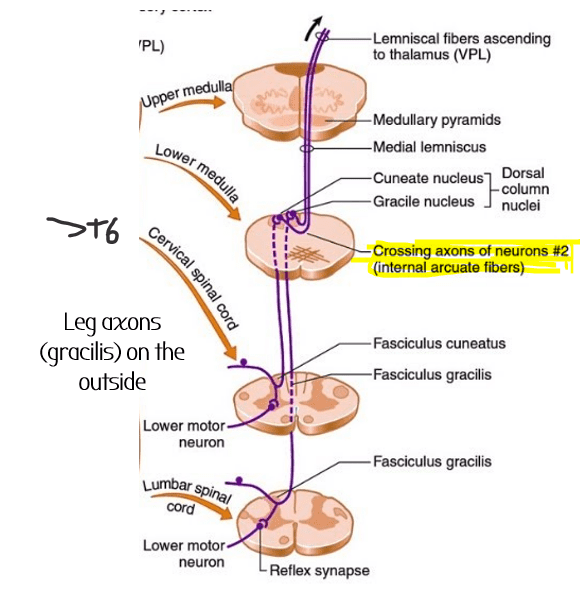
Fibres go to the VP nucleus of the thalamus –> S1 somatosensory areas via reciprocal connections.
Vibration & Proprioception
-test vibration using a 128Hz tuning fork 🍴 in sensory exam
-test proprioception by pushing big toe either up or down and asking patient to tell you which way its moving.
Crossed at the medulla in brainstem
• TABES DORSALIS – most common form of neurosyphilis – stamping gait due to lack of proprioception in dorsal column
• FRIEDREICH’S ATAXIA: genetic degenerative of DC tracts & spinocerebellar tracts
•STROKES:
ACA (contralateral leg🦵),
MCA (contralateral face 😮/ arm 💪),
Brown-Sequard Syndrome – bilateral at level of lesion, ipsilateral below the lesion
Not affected in VSA stroke / syringomyelia 🙂
Trigeminal Touch Pathway
Pathway
Trigeminal nerve (V). Projects to PRINCIPAL/CHIEF SENSORY NUCLEUS
- Then crosses at midline, joins medial leminsical pathway
- Then projects to Ventral posterior (VP) nucleus in thalamus just like DCMLP (but more medially in the nucleus)
- Then projects onto S1
Same as dorsal column but for the face
Crosses at midline from cheif sensry nucleus
Pain fibres
C | Smallest | Pain, itch, temperature |
Ad | Larger | Fast pain, temperature |
AB | Even larger | Skin mechanoreceptors, touch |
Aa | Largest | Proprioceptors |